Swallow Function in Advanced Age
 Swallow Function in Advanced Age
Swallow Function in Advanced Age
Age-related changes in swallow function are observed starting at approximately age 60; by age 80, most individuals will experience some degree of age-related swallow changes (presbyphagia) (Iannuzzi-Sucich, Prestwood, & Kenny, 2002). As an individual ages, there are alterations in sensory function, the musculoskeletal system, and the neural system. These age-related changes may impact swallow function. However, a healthy elderly individual can produce a functional swallow despite presbyphagia. Regardless, these changes put an older individual at risk for dysphagia. Box 1.50 shows a VFES of a healthy elderly individual. Box 1.51 displays areas of decline associated with advanced age.
Box 1.50 External Link
Box 1.51: Schematic of the impact of advanced age on swallow function
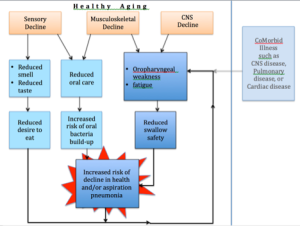
Anatomically, changes in dentition, ossification of cartilage, presence of arthritis, or loss of muscle fibers, muscle tone, or muscle strength are all associated with advanced age. These anatomical alterations impact swallow physiology. Identification of these age-related changes must be teased out from a population with an increased risk of diseases (co-morbidities) that may be related to dysphagia. Further, the healthy aging adult may not report alterations to swallow function due to the slow rate at which these changes occur. Thus, age-related physiologic changes to swallow function might be detectable only to the professional or with instrumental evaluation, especially if there is no obvious impact on general nutrition or hydration.
Clinical Note
The geriatric population as a whole, not just those with dysphagia, are at risk for dehydration due to changes in the thirst response and decline in kidney function (Mentes, 2006). Elderly individuals should be reminded that good hydration correlates with better health, including improved outcomes in orthopedic rehabilitation (Mukand, Cai, Zielinski, Danish, & Berman, 2003).
Dentition
Dentition can change with respect to the number of teeth, or the general health and condition of teeth. The number of permanent teeth present in the mouth of a geriatric patient can range from full to partial dentition, to complete absence of teeth (edentulous). Although poor dentition may be compensated for with partial or full prosthetic dentures, these cover the gum tissue reducing sensory input. When prosthetics are used, the fitting can vary from well-fitted to free-floating. Dentures that are poorly supported due to periodontal disease or inadequate oral bone structure may not aide mastication and swallowing as effectively as intended. Altered dentition, which is common in geriatric individuals, can impact eating habits, food selection, mastication, and bolus control during the oral phase of the swallow (Fucile et al., 1998; Shtereva, 2006; Yoshikawa et al., 2006).
Clinical Note
Poorly fitted dentures can cause difficulty with mastication and bolus control. Dentures should be checked for fit, especially after a medical event, such as stroke.
Joint & Cartilage Changes
With age there is increased incidence of arthritis in joints and ossification of cartilage (Casiano, Ruiz, & Goldstein, 1994). Because the larynx contains both, these changes may impact the behavior of the larynx during the swallow. As cartilage ossifies it becomes heavier. A heavier larynx may have a lower rest point and require greater muscle strength for lifting. Arthritis can impact laryngeal joints, which may change the airway protection mechanism. Arthritis may also affect the cervical spine reducing the ability of the head to move as needed during food entry into the oral cavity or transport of food into the pharynx. Further, arthritis in the cervical spine may result in alterations in the vertebral shape eventually impinging on the pharyngeal space. Osteophytes or bony spurs, which are bony outgrowths associated with joint degeneration, are observed somewhere on the spine in all individuals over the age of 80 (Hilel, 1962) (Box 1.52). Although osteophytes are typically asymptomatic, it is possible for an osteophyte to become large enough to compress the oropharynx and interfere with swallowing (Lee, Bae, & Paik, 2014; Lee, Kim, & Paik, 2008; Papadopoulos, Chen, Feldenzer, Bucci, & McGillicuddy, 1989; Strasser et al., 2000). Also, a small well-positioned osteophyte can alter bolus flow toward a detrimental path.
Box 1.52: Cervical spine changes
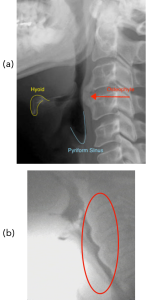
A. anterior cervical osteophyte
B. Scalloped image reflecting cervical spine degeneration.
Muscle Fiber Changes
Muscles change with age either with respect to the number of fibers (reducing the cross sectional area of the muscle) or fiber type. Loss of muscle fibers due to disuse atrophy or sarcopenia may render muscles weaker (Burkhead, Sapienza, & Rosenbek, 2007; Easterling & Robbins, 2008; Kim & Sapienza, 2005; Robbins et al., 2005). In addition, conversion of a fiber type may change the performance ability of a muscle (Monemi, Liu, Thornell, & Eriksson, 2000). Changes in fiber composition have been observed in oral, pharyngeal and laryngeal muscles (Rodeño, Sánchez-Fernández, & Rivera-Pomar, 1993). The tongue, a muscular hydrostat important in efficient swallowing, shows reduced strength and increased tongue fat (about 2.7% per decade) with increased age (Nicosia et al., 2000; Rother, Wohlgemuth, Wolff, & Rebentrost, 2002).
Clinical Note
There is evidence that swallowing can be improved with muscle strengthening tasks. We should consider the oral and pharyngeal muscles much the way we think about the big muscles in the body with respect to routine exercise. The best exercise for swallowing is swallowing. Even in the oral and pharyngeal cavity, if you don’t use it, you lose it. If you want to know more, consider reading Robbins et al., 2005.
Overall, age-related changes in oropharyngeal muscles result in slower, weaker, and less dynamic movement of the swallow structures (reduced kinematics). Specifically, the weaker muscles may be inadequate to motivate the ossified (i.e., heavier) larynx out of the way of the bolus flow in a timely or complete fashion. The weaker muscles will generate a less enthusiastic pressure, reducing driving force on the bolus throughout the swallow. The reduced pressure generation throughout the swallow increases the risk of penetration of material into the airway and residue of material in the pharynx after the completion of the swallow.
Historically, changes in muscle function have been considered an aspect of normal aging. However, recent data supports that a regular fitness routine may thwart much of the muscle fiber changes considered to be part of normal aging. Studies focused on tongue strengthening have shown promising results (Kletzien, Russell, Leverson, & Connor, 2013).
Aging has been associated with reduced oral intake, which results in a reduction in mealtime related oral and pharyngeal muscle exercise. This reduced exercise may further exacerbate age-related muscle weakness. Reduced oral intake also introduces other issues, such as poor nutrition and dehydration, both of which can lead to additional problems, such as weight loss, loss of energy, or constipation.
When considered in combination with joint degeneration, age-related muscle changes produce a slower, weaker swallow. Any alteration that changes structural movement or pressure generation on the bolus can reduce the successful and efficient transfer of the bolus from the oral cavity to the esophageal body. For example, ossification of cartilage increases the weight of the larynx. Thus, greater muscle effort may be required to maneuver the hyo-laryngeal elevation needed during safe swallow. If greater muscle function is not available, as may be the case in aging individuals, reduction in hyo-laryngeal trajectory can alter airway protection by keeping the airway in the path of the bolus, and reducing epiglottic down-folding and UES opening.
Functional Reserve
Functional reserve is the remaining capacity of a physiologic system after it has fulfilled a required function. For example, in swallowing you may need 40 kPa of tongue-to-palate pressure to swallow a typical bolus. Yet, your tongue can produce a maximum of 65kPa. The difference between the maximal ability and the required threshold to complete a task is the functional reserve. This reserve is called upon when the system is required to perform a more vigorous output. It may also be used when the system is fragile or perturbed. As reserve declines, so does the functional ability to perform tasks and cope with perturbations. Box 1.53 provides a schematic of how declining reserve can occur with advanced age and disease.
Box 1.53: Schematic of functional reserve
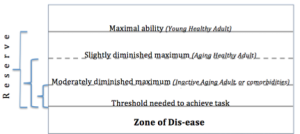
Functional reserve is reduced with age. That means that the physiologic redundancy and excess ability are no longer available to aid the system during periods of physiologic stress (such as the presence of illness), or perturbation to the system (such as an oddly textured or shaped food, or presence of a tracheostomy tube). Muscles with reduced functional reserve may inadequately motivate a large or more viscous bolus that requires greater than average muscle effort. In the face of declining functional reserve, smaller physiologic challenges can compromise swallow function.
A Note About Frailty
There is much debate about frailty in aging. An operational definition proposed by Fried and colleagues (2001) includes meeting 3 of the following 5 criteria: reduced hand grip strength, reduced energy, reduced walking speed, low physical activity, or unintentional weight loss. Frailty may be a reflection of reduced muscle mass and functional reserve across physiologic systems. As such, a frail individual will be prone to decline when exposed to stressors (Fried et al., 2001). Historically, frailty was considered a normal aspect of aging. However, it is now gaining support as a medical syndrome that can be largely avoided with proper exercise (Xue, 2011). (Frailty is discussed in greater detail in chapter 2.)
Polypharmacy
Polypharmacy is the use of multiple medications. The increased incidence of polypharmacy in aging may impact swallow function. While the drug companies provide a list of side effects for an individual drug, they do not address the interaction of one medication on another. For adults between the ages of 75 and 85 who live independently, approximately 37% take at least five different medications (Qato et al., 2008). This number does not reflect over-the-counter medications or supplements that may also be consumed. For adults residing in nursing homes, the number of different medications is typically greater than five. For more than half of these individuals, at least one prescription is deemed unnecessary. Adverse drug effects and drug interactions increase with the number of medications taken. Polypharmacy is linked to reduced functional reserve and increased cognitive deficits, and 50% of individuals who take at least 10 medications present with malnutrition (Jyrkkä, Enlund, Lavikainen, Sulkava, & Hartikainen, 2011).
Esophageal Changes
Presbyesophagus refers to age-related changes in esophageal peristalsis. Although not a consistent finding, with age the duration of esophageal peristalsis may increase (take longer) and the amplitude of esophageal peristalsis may decrease (become less vigorous) (Hollis & Castell, 1974; Robson & Glick, 2003). Esophageal sphincter tone (both upper and lower) reportedly reduces with age. Hence, there is an age-related increase in reflux (DeVault, 2002). As these esophageal changes may cause discomfort during eating (e.g., non-cardiac chest pain; Richter, 2000), they may alter an individual’s food choices or desire to eat.
Clinical Note
It is difficult to differentiate if changes in esophageal function are related to advanced age or are the result of illnesses and diseases that increase with advanced age.
Neurophysiology
In addition to changes in physiology, there are age-related alterations in neurophysiology (Rossini, Rossi, Babiloni, & Polich, 2007; Russ, Gregg-Cornell, Conaway, & Clark, 2012). A slower, weaker swallow may be related not only to reduced muscle function (sarcopenia), but to reduced neural drive. With advanced age there are decreased nerve conduction velocities and reduced levels of neurotransmitters (Weismer & Liss, 1991). In related research, there is evidence of reduced firing rate in laryngeal muscles during phonation (Luschei, Ramig, Baker, & Smith, 1999; Takeda, Thomas, & Ludlow, 2000). It is plausible that neural drive may also be reduced in the oropharyngeal muscles during swallowing. This slower, weaker swallow leads to less dynamic range in the pharyngeal structures, which impacts the timing, extent, and duration of hyo-laryngeal trajectory and UES opening. This increases the potential for penetration and aspiration, and pharyngeal residue after the swallow (Daniels et al., 2004; Robbins, Coyle, Rosenbek, Roecker, & Wood, 1999).
Sensory Function & Trigger Site for Pharyngeal Swallow
Oropharyngeal sensory function declines with age which may alter the timing and location of the pharyngeal swallow trigger (Aviv, 1997; Aviv et al., 1994). That is, in healthy aging individuals, there is evidence that the trigger site lowers with age. As the trigger site lowers to the level of the vallecula or the pyriform sinus, the airway remains exposed while the bolus traverses the pharynx awaiting a swallow response. This results in an increased risk of penetration and aspiration before the swallow.
Respiratory Changes with Age
Respiratory structure can change with age impacting the physiologic function of blood oxygenation. With age, the rib bones may become thinned and the lungs less elastic. Further, the spine alignment may be altered and not supportive of maximal lung inflation. Ciliary activity becomes less efficient, reducing oxygen uptake. These aspects, combined with potentially age-related muscle weakness in the respiratory muscles, may result in reduced lung volumes and reduced efficiency during gas exchange. Further, respiratory diseases that increase in frequency with age can also result in poor gas exchange. Because respiration and swallowing share a conduit, during the swallow, gas exchange is halted for a brief period (respiratory cessation) to allow the air tube to become a food tube. However, if gas exchange is inadequate (individual has low oxygen saturation in blood), the respiratory center may supersede the swallow center by imposing restrictions on the duration of respiratory cessation. The resulting shortened deglutitive apnea impacts the timing of the swallow and increases the risk of penetration and aspiration. This is concerning, especially considering that these events occur in a lung that may be less able to handle the insult of aspiration.
“Want more?”
The 3rd leading cause of death in elderly individuals in the US is chronic obstructive pulmonary disease (COPD). You can learn more about the disease in this youtube video and you can learn more about the impact on swallowing by checking out this article Dawod, Thao, Ward, & Luraschi-Monjagatta, 2016.
Salivary Function and Taste Reception
Salivary flow decreases and xerostomia (dry mouth) increases with age (Christensen, Petersen, & Steding-Jessen, 2007; Ship, Pillemer, & Baum, 2002; Flink, Bergdahl, Tegelberg, Rosenblad, & Lagerlöf, 2008). This may be due to (1) increased use of medications that reduce salivary flow, (2) reduced liquid intake or a “nothing by mouth” status, (3) reduced levels of awareness that may be accompanied by mouth breathing, particularly when sleeping in an upright position, such as napping in a chair, or (4) changes in the function of the salivary glands. Regardless, xerostomia may require individuals to use more effort during swallowing.
“Want more?”
Learn more about the impact of advanced age on saliva flow by reading Smith et al., 2013.
Reduction in saliva also impacts oral health, taste function, food break down, and bolus development. Saliva contains protective enzymes to help reduce oral bacteria. With reductions in saliva there is an increase in dental decay and bacteria buildup in the oral cavity. Thus, if aspiration of saliva should occur, the saliva bolus is infused with a higher amount of bacteria. Consistent and frequent oral hygiene may help reduce the effect of the reduced saliva.
As saliva carries enzymes that begin the break down of food during mastication, reduced saliva will eliminate some of the early break down of food. Further, during mastication, reduced saliva will alter the saliva ratio in the bolus. This may alter the cohesion of the bolus during development making it more likely that particles may separate from the main bolus during transit through the oral or pharyngeal cavity.
Although some geriatric individuals complain of loss of taste, there is limited evidence to support loss of taste function. It is possible that some of the reported loss of function is related to a decline in olfactory functions. However, reduction in saliva or changes in the ion transport may also play a role (Mistretta, 1984). Taste receptors are chemoreceptors that require some degree of saliva to secure ion transport. Therefore, reduced saliva may alter the transport of chemical solutions through the ion channels of the taste cell membrane (Mese & Matsuo, 2007).There are other age-related events that may cause changes in taste. The presence of dentures may lead to a change in taste due to reduced oral surface exposure. Geriatric individuals are more likely to be on medications, and many medications can alter taste function. Further, because the ability to perform adequate oral hygiene may decrease with age, an individual may have altered taste from the residue and bacteria left behind from inadequate oral hygiene, effectively altering incoming tastes.
Clinical Note
For individuals at risk for aspiration, good oral hygiene reduces the risk of aspiration pneumonia.
Oral Hygiene
Despite the fact that good oral hygiene is linked to lower incidence of illness in frail and elderly individuals, the ability to perform oral hygiene tasks declines with age (Christensen et al., 2007). This may be due to reduced fine motor function, reduced vision and poor eye-hand coordination, or changes in cognition or mental status. Altered dentition (i.e., presence of dentures) requires different approaches to oral hygiene that may be difficult for the elder individual to achieve. A thorough and consistent oral hygiene routine is linked to reduced oral bacteria and improved health. In fact, in a study of causes of aspiration pneumonia, poor oral hygiene was an important predictive factor (Langmore et al., 1998).
Cognitive Decline
The literature is replete with the dos and don’ts of aging to avoid loss of cognitive function. However, all individuals, if graced with long life, will eventually experience some degree of cognitive decline. Regardless, in healthy aging, limited cognitive decline does not greatly impact swallow physiology. However, cognitive decline may play a role in reduced oral intake or ability to comply with denture wearing (Furuta et al., 2013; Steele, Greenwood, Ens, Robertson, & Seidman-Carlson, 1997). These mealtime difficulties are particularly prevalent in institutionalized elderly with cognitive decline (Steele et al., 1997). The impact of more significant cognitive decline, such as dementia, is not an aspect of healthy aging, and, therefore, is not discussed in this section.
Social and Quality of Life
Aging individuals may have reduced social interactions thereby altering quality of life. Age-related alterations in swallow function may further reduce socialization due to embarrassment or fear. However, for most healthy aging individuals with presbyphagia (not dysphagia), this is not a typical outcome. Alterations to swallow function that impact socialization are more typically associated with disease-related dysphagia rather than presbyphagia. Two studies that looked at quality of life in healthy elderly versus elderly with disease showed that despite minor changes in swallow function in the healthy aging population, quality of life scores were not impacted in the healthy elderly (Leow, Huckabee, Anderson, & Beckert, 2010; Palmer, Neel, Sprouls, & Morrison, 2010). However, if reduced social interaction and increased isolation occur due to changes in swallow function, quality of life may be reduced.
Summary
The combination of all these anatomic and physiologic alterations may result in a more sluggish, less robust swallow, yielding longer transit times with weaker muscle contractions and reduced dynamic range of physical structures. In the worst case scenario, the end result is reduced swallow capacity, reduced bolus control, reduced bolus transit, increased pharyngeal pooling and residue, and reduced airway protection. While the slower, weaker swallow may be related to increased muscle weakness and reduced neural drive, it has also been postulated that, to some degree, the slower rate of swallow may be a compensatory strategy used by healthy aging individuals to improve pressure generation during a swallow (Robbins, Levine, Wood, Roecker, & Luschei, 1995). A weaker swallow can be compensated for by slowing down the swallow to give more time to build up strength for the swallow. The reduced swallow capacity noted with age may also be a compensatory strategy to deal with the weaker swallow (Nilsson, Ekberg, Olsson, & Hindfelt, 1996).


