Pharyngeal Cavity
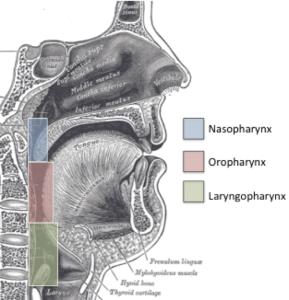
The pharyngeal cavity is a fibro-muscular tube that can be divided into three regions: the nasopharynx (the part behind the nose), the oropharynx (the part behind the mouth), and the laryngopharynx (a.k.a. the hypopharynx, the part behind the larynx) (Box 1.22). The tube has several gates or valves — an opening into the nasal cavity through the velopharyngeal valve, an opening into the oral cavity through the lingual-velar valve, an opening into the airway through the laryngeal aditus, and an opening into the esophagus through the upper esophageal sphincter (UES, also known as the pharyngo-esophageal segment). Other structures of interest in the pharynx include the base of tongue and the epiglottis.
Box 1.22. Regions of the Pharyngeal Cavity
Box 1.23. Pharyngeal Spaces
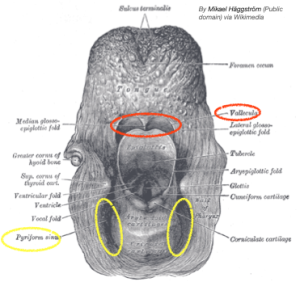
Pharyngeal Spaces
If pharyngeal structures have not been altered by age or disease, there are two spaces in the pharynx where food or liquid may rest (Box 1.23). In the laryngopharynx, the juxtaposition of the epiglottis with the base of tongue, at the point of the hyoid bone, creates a pocket known as the vallecula space. (Note: Vallecula are crevices that can be located throughout the body. We are interested in the vallecula in the pharynx.) This space is mostly obliterated during the swallow when the epiglottis inverts.
On either side of the thyroid lamina there are sinus cavities known as the pyriform sinuses. These two pockets sit just superior to the upper esophageal sphincter (UES). Adequate UES opening and timing of the opening, combined with sufficient pharyngeal pressure, will keep the pyriform sinuses relatively free of bolus after the swallow is complete.
Clinical Note
If the pressure in the inferior pharynx increases and the CP muscle neglects to relax in time, the increased pressure at the intersection between the two muscle bellies of the IPC can be easily dissected. The resulting pocket is referred to as Zenker’s Diverticulum. Watch the video below and note the Zenker’s indicated with a red arrow.
Pharyngeal Muscles
The pharyngeal tube contains three important constrictor muscles: superior pharyngeal constrictor (SPC), middle pharyngeal constrictor (MPC), and inferior pharyngeal constrictor (IPC) muscles (Box 1.24). The SPC muscle has multiple insertion points; this muscle goes from the pterygoid-mandibular raphe to the pharyngeal raphe and root of the tongue. The action of the SPC is to collapse the upper part of the pharyngeal tube. The inferior fibers of the SPC muscle make up the glossopharyngeal muscle. The MPC muscle goes from the hyoid bone to the medial pharyngeal raphe. The SPC and MPC muscles are innervated by the pharyngeal plexus.
Box 1.24. Pharyngeal muscles
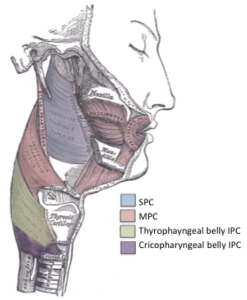
The IPC muscle goes from the medial pharyngeal raphe to the thyroid and cricoid cartilages. Thus, IPC muscle is comprised of two muscle bellies. The upper fibers which originate from the thyroid cartilage is the thyropharyngeal belly of IPC. Both bellies insert on the medial pharyngeal raphe. The upper fibers of the IPC collapse the lower pharynx and are innervated by the superior laryngeal branch of CN X. The lower fibers which originate from the cricoid cartilage are referred to as the cricopharyngeal (CP) belly. Although anatomically considered to be part of the IPC muscle, the most inferior bands of the IPC, the CP muscle, functionally behaves as a separate muscle during swallowing, and therefore, will be considered as such in this text. Unlike other muscles of swallowing, as noted in Box 1.25, the CP muscle is tonically active and turns off during the swallow.
Box 1.25: EMG of the CP muscle and submittal muscles during a swallow.
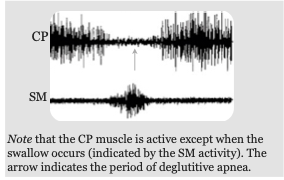
Collectively, the SPC, MPC and upper fibers of the IPC work to squeeze the pharynx from top to bottom and collapse the pharyngeal tube onto the tail of the bolus providing impetus for bolus propulsion. The CP muscle, which is tonically active, i.e., always contracted, relaxes during the swallow to allow passage of the bolus from the pharynx into the esophagus. It is innervated by CN X.
Box 1.26 Image Gallery: Gallery of longitudinal pharyngeal muscles
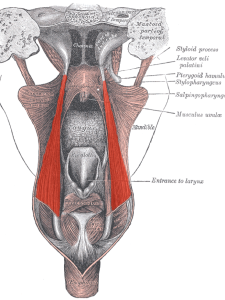
Salpingopharyngeus Muscle
(By Uwe Gille, modified from Gray1028.png, Public Domain.)

Stylopharyngeus Muscle
(Public Domain, https://commons.wikimedia.org/w/index.php?curid=1607066)
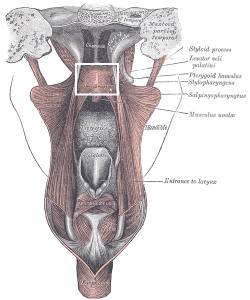
Palatopharyngeus Muscle
(Public Domain, https://commons.wikimedia.org/w/index.php?curid=1607066)
Deep to the constrictor muscles are long muscles that, when contracted, elevate and thereby shorten the pharynx. The stylo-pharyngeal muscle goes from the styloid process of the temporal bone and inserts onto the thyroid cartilage (Box 1.26). In addition to elevating and shortening the pharynx, the stylopharyngeal muscle may help with pharyngeal dilation needed during swallowing of a large bolus. It is innervated by the muscular branch of CN IX.
The palatopharyngeal muscle (discussed previously) travels from the soft palate to the pharynx at the level of the thyroid cartilage. Superior to the insertion point, interaction of fibers from both sides sometimes result in an obvious muscular prominence referred to as Passavant’s Ridge. In conjunction with mucous membranes, this muscle forms the palatopharyngeal arch (aka posterior faucial pillar). It is innervated by fibers from CN XI and the pharyngeal branch of CN X.
Innervated by the pharyngeal plexus, the salpingo-pharyngeus muscle starts in the auditory tube (near the eustachian tube) and merges with the palatopharyngeus. Upon contraction, it elevates the larynx and pharynx. It is also involved in opening the eustachian tubes. Collectively, these long pharyngeal muscles elevate and shorten the pharynx during the swallow, effectively shortening the transit time through the pharynx by shortening the length of the pharyngeal tube.
UES
At the bottom of the pharyngeal tube is the upper esophageal sphincter (UES) region or the pharyngo-esophageal (PE) segment. It is a 2 to 4 cm region made up of mucosa, elastin, collagen, and muscle fiber. The muscle in this region, the cricopharyngeus muscle, is tonically contracted (receives continuous neural drive resulting in constant muscle activation). While at “rest” (not swallowing), there is a high resting pressure in the region with increased pressure noted during gagging and Valsalva maneuver. This closure prevents back-flow of contents from the esophagus into the pharynx. It is innervated by the pharyngeal branch of CN X.
Clinical Note
UES opening during the swallow is achieved through active (relaxation of the CP muscle) and passive forces (mechanical traction from hyo-laryngeal elevation).
Clinical Note
 Deficits in UES opening can be related to the duration of opening or the extent of opening. These aspects can be visualized on VFES. An example of reduced extent of UES opening is a “CP bar”.
Deficits in UES opening can be related to the duration of opening or the extent of opening. These aspects can be visualized on VFES. An example of reduced extent of UES opening is a “CP bar”.
Clinical Note
If the UES does not adequately open, then material may stay in the pyriform sinus putting the patient at risk for aspiration after the swallow.
During a swallow, the CP muscle relaxes (temporary cessation of neural discharge). Reduced activation is also noted during sleep, smoking, or ingestion of alcohol, chocolate, mint, fried or fatty foods, or caffeine, as well as during belching or vomiting. The opening of UES is governed not only by these active muscular forces of the cricopharyngeus muscle, but also a passive traction force. The fibers of the UES region are attached to the back of the larynx (cricoid cartilage). Thus, when muscle forces elevate the larynx, the linkage between cricoid cartilage and the UES translates to a mechanical pull on the UES. Note that the posterior fibers of the UES are anchored to the posterior pharyngeal wall. Specifically, the anterior aspect of the UES is pulled up and forward with laryngeal elevation. Pulling open the UES results in a reduction of the resting pressure. The combination of the muscular relaxation and the upward anterior traction result in opening of the UES region to allow for passage of the bolus from the pharynx to the esophagus. When closed, the UES region eliminates back-flow from the esophagus into the pharynx. Finally, the UES prevents air from entering the esophagus.

