Oral Cavity
Lips
The lips, when opened, afford entrance of the liquid or food into the mouth. When closed, the lips, in conjunction with the front teeth and jaw, provide an anterior containment system so food or liquid does not escape. Anatomically, the lips can be divided into the upper and lower lip. Box 1.2 includes common anatomical markers of the lips.
Box 1.2 Image Gallery: Lip Anatomy
The orbicularis oris, a four quadrant, sphincter-like muscle with fiber attachments at the oral commissure, is the primary muscle of the lips (Box 1.3). It is a complex muscle composed of fibers from various facial muscles, as well as fibers specific to the lips. Collectively these fibers can result in lip rounding, protruding, opening, or closing. Motor innervation to the orbicularis oris comes from CN VII, which is innervated from the contralateral side; sensory innervation comes from CN V from the contralateral side. The muscular action of the lips results from the combined actions of the orbicularis oris and other muscles in the perioral region. While these perioral muscles play a role in the muscular positioning of the lips for articulation, the important actions for swallowing include opening to allow entrance of food or liquid, and closing, with some degree of contact, to maintain a seal against anterior leakage. Lip rounding or closure, an action needed to ensure anterior bolus containment, should be symmetrical from all four quadrants (upper right, lower right, upper left, lower left).
Box 1.3: Orbicularis Oris Muscle
Clinical Note
- Weakness in the lips may result in drooling during mealtimes. Chronic drooling may be the result of weak lips in conjunction with overproduction or poor management of saliva including reduced saliva swallow frequency.
- An open lip posture may be indicative of lip weakness or poor nasal patency.
- When asymmetrical lip movement is observed, it implies that there is either contralateral cortical damage or ipsilateral nerve damage.
Want more?
Muscles of importance that insert into the oral commissure of the lips (where the upper lip and lower lip intersect) include the buccinator, levator anguli oris, depressor anguli oris, zygomaticus major, and risorius. Surrounding perioral muscles that insert into the upper lip include the levator labii superioris, levator labii superioris alaeque nasi, and zygomaticus minor. Perioral muscles that insert into the lower lip include the depressor labii inferioris, mentalis, and platysma.
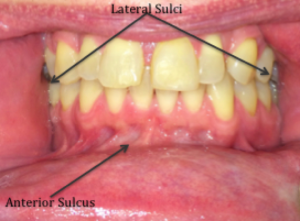
Cheeks

The cheeks provide lateral containment of food and liquid in the oral cavity. This is partly due to the mere presence of the structure, and partly from active contraction of cheek muscle. This contraction provides support to keep material out of the lateral sulci (cheek pocket) and help increase and direct oral pressure.
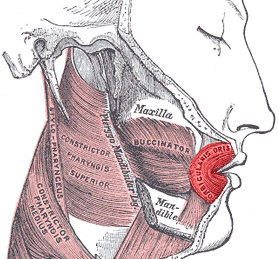
The external surface of the cheek is covered with skin; the internal surface is covered with a mucous membrane. The primary muscle of the cheek is the buccinator muscle, which when contracted can provide lateral tension in the oral cavity (Boxes 1.4 & 1.5). Anteriorly, the fibers of this muscle interdigitate with the muscles of the upper and lower lip at the oral commissure. Posteriorly, the buccinator muscle interdigitates with the superior pharyngeal constrictor muscle. Motor innervation to the buccinator muscle comes from the buccal branch of CN VII; sensory innervation comes from CN V.
Box 1.4 Image Gallery: Buccinator Muscle
| By Henry Vandyke Carter [Public domain], via Wikimedia Commons |
By Otto Placik (Own work) [CC BY-SA 3.0 ) via Wikimedia Commons |
Box 1.5 Video: Buccinator Muscle
Deep to the musculature of the cheek are fat pads (Box 1.4). In infants the buccinator muscle, along with the fat pads, assists in stabilizing the nipple for sucking. Due to advances in facial reconstruction, the anatomical structure of the buccal fat pads has been well defined (Zhang, Yan, Qi, Wang, & Liu, 2002). While three discrete lobes can be identified, it is the intermediate lobe that is implicated in providing support during infant sucking. This lobe of the fat pads is prominent at birth, and typically shrinks by 1 year of age. It is possible that the prominence of this fat pad may linger in individuals who are long-term finger suckers. It is speculated that the other lobes of the buccal fat pads provide a life-long protective layer over fragile facial muscles.
Clinical Note
Reductions in buccal tension can lead to reduced oral pressures and increased risk of residue in the lateral sulci.
Clinical Note
The facial nerve innervates both sides of the upper face, but only the contralateral side of the lower face. That means that the right hemisphere provides the only motor innervation to the left lower face (and visa versa). So a unilateral stroke may result in no observable asymmetry in the upper face, but weakness in the lower face of the opposite side. If you see weakness on the same side in both the upper and lower face, suspect a nerve injury.
Clinical Note
 Finger sucking can result in alterations to the oral cavity including an increase in palatal arch and a decrease in palatal width, as well as malocclusions and proclinations of the maxillary and mandibular incisors (Larsson, 1972; Moimaz et al., 2014).
Finger sucking can result in alterations to the oral cavity including an increase in palatal arch and a decrease in palatal width, as well as malocclusions and proclinations of the maxillary and mandibular incisors (Larsson, 1972; Moimaz et al., 2014).
Palate
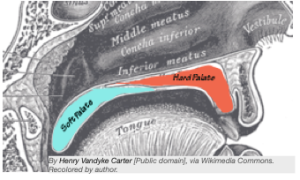
The palate or roof of the mouth can be divided into the hard palate (the front part) and the soft palate (the back part) (Boxes 1.6 & 1.7). The membrane-covered bony structure, or hard palate, serves as the roof of the mouth and separates the oral and nasal cavity. The intact hard palate provides superior containment for food or liquid. It also serves as a contact surface to press against when masticating a bolus.
The palate is fairly flat at birth and becomes arched as the infant develops. The height and width of the arch, sometimes referred to as the palatal vault, can vary across the lifespan and the population. Although a high, narrow arch is considered within normal limits, it may be indicative of a history of finger sucking or perhaps associated with a syndrome.
Box 1.6 Hard and Soft Palate
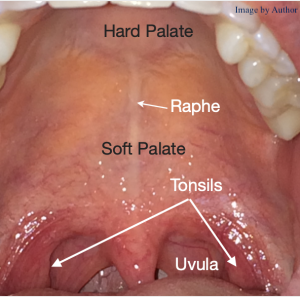
Box 1.7 Hard and Soft Palate
Clinical Note
Alterations to the palate may impact the break down of food, as well as the superior containment of food.
Clinical Note
When a palate is congenitally open
it is referred to as a cleft palate.

Clinical Note
Orthodontic approaches for altering the size and shape of the palatal vault are best completed prior to closure of the mid-palatal suture, which occurs between 12-15 years of age in most individuals (Proffit & Fields, 2000).
Clinical Note

Although usually asymptomatic, palatal tori may be problematic when fitting an individual for upper dentures, indirectly interfering with mastication. In cases where the presence of the palatal tori impacts function, surgical removal may be considered.
Box 1.8 Soft palate during the swallow.
 |
 |
| Image 1: The soft palate as part of the lingual-velar valve. Note the nasal airway is open. |
Image 2: The velum makes contact with the posterior pharyngeal wall (velar-pharyngeal valve), closing the nasal cavity. |
Original by Hellerhoff and modified by Anka Friedrich (CC BY-SA 3.0)
The oral surface of the hard palate is slightly rough with visual ridges called palatal rugae (Box 1.7). These ridges may assist during mastication by providing a rigid rough surface on which to compress the bolus. At the midline of the hard palate there is a visible raphe. At times, a visible protrusion or palatal torus is observed at midline. Palatal tori are slow-growing bony outgrowths that can vary in size and appearance. Its prevalence ranges from 12% to 26% in the general population (García-García, Martínez-González, Gómez-Font, Soto-Rivadeneira, & Oviedo-Roldán, 2010). While the presence of palatal tori may alter oral pressure measurements and mastication patterns, they are typically asymptomatic with respect to swallowing. Clinical examination of the hard palate should mention any notable height or shape variations.
Want more?

Inspection of the soft palate may reveal a bifid uvula (a uvula that is split in two). This is an important observation, as it may serve as a marker for other anomalies such as a sub-mucous cleft (Shprintzen, Schwartz, Daniller, & Hoch, 1985).
“Want more?”
A high, narrow palatal arch is associated with several syndromes including Crouzon syndrome, Down syndrome, Apert syndrome, Treacher-Collins syndrome, Marfan syndrome, Incontinentia Pigmenti, Pierre-Robin syndrome, Turner’s syndrome, Noonan syndrome, and Cardiofaciocutaneous syndrome.
Clinical Note
ADD WHATEVER TEXT.
Abutting the hard palate posteriorly is the soft palate (also known as the velum), which as the name implies, is the soft muscular aspect of the palate. The “punching bag” at the terminal end of the soft palate is referred to as the uvula. For swallowing, the soft palate serves as a door that when lowered and approximated with the base of the tongue, serves as part of the lingual-velar valve to provide posterior containment of food or liquid during bolus development and oral transport (Box 1.8). When elevated, the soft palate serves as the active component in the velar-pharyngeal valve, which seals the nasal cavity during the pharyngeal phase of the swallow and prevents liquid or food from entering the nasal cavity.
“Want more?”
What is the pharyngeal plexus?
The pharyngeal plexus is a nerve that is formed by fibers from both CNs IX and X. Some authors also include fibers from CN XI in their description of the pharyngeal plexus.
Clinical Note
Muscles of the soft palate receive bilateral input from the cortex due to the bilateral upper motor neuron innervation of CN V. Therefore, asymmetrical movement implies a lower motor neuron lesion
Clinical Note
If the levator veli palatini muscle contracts only on one side, the soft palate will be pulled in a lateral direction pointing to the incompetent side.
Opening and closing of the velar-pharyngeal space is accomplished by multiple small muscles that work together to elevate, press, and depress the velum to and from the posterior pharyngeal wall during the swallow. Muscles that elevate the soft palate include the levator veli palatini and uvular muscles. The levator veli palatini muscle, which makes up much of the bulk of the velum, goes from the temporal bone to the soft palate. When contracted, it moves the velum in a superior and posterior direction making contact with the posterior pharyngeal wall. The uvular muscle goes from the soft palate to uvula; when contracted it shortens and lifts the soft palate. Elevator muscles of the soft palate receive motor innervation from the pharyngeal plexus (Ezzat & El-Shenawy, 2015), which is composed of a network of nerve fibers from cranial nerves IX, X, and XI. Although not considered a soft palate muscle, the superior pharyngeal constrictor muscle plays a role in the closing of the velar-pharyngeal valve.
“Want more?”
In healthy individuals, the palatal vault of adult males is typically higher and wider than in females (Ahmad, 2009); in children, girls’ palatal vaults are narrower than boys’ (Tsai & Tan, 2004).
Clinical Note
Weakness or poorly timed contraction of the palatoglossus muscle may result in poor posterior containment leading to premature spillage of oral material into the unsuspecting pharynx. That is, material enters the pharynx while the airway is unprotected. This puts an individual at risk for aspiration before the swallow.
The tensor veli palatini muscle does not necessarily assist in opening or closing the velum during the swallow. However, upon contraction, the tensor veli palatini muscle, which goes from the sphenoid bone on the medial pterygoid plate to the soft palate, tenses the soft palate and may assist in opening the eustachian tubes. It is innervated by CN V.
Depression of the velum is likely related to the inaction of velar elevator muscles with active assistance from the palatoglossus and palatopharyngeus muscles. The palatoglossus muscle, housed within the anterior faucial pillar, goes from the soft palate to the sides of the tongue. When contracted it pulls the back of the tongue up and/or pulls the soft palate down toward the tongue. This helps facilitate posterior containment of food in the oral cavity while the bolus is being prepared. The palatopharyngeus muscle, housed within the posterior faucial pillar, goes from the soft and hard palate to the pharyngeal wall. When contracted, this muscle pulls the pharynx superiorly, effectively shortening the length of the pharyngeal tube. These are both innervated by fibers from the CN X, specifically the pharyngeal plexus (Ezzat & El-Shenawy, 2015).
Teeth

The development of baby teeth begins in utero, but they do not erupt through the gums until approximately 6 months of age. Baby teeth are also referred to as primary teeth, deciduous teeth, or, less popular, milk teeth. There are 20 primary teeth—four central incisors, four lateral incisors, four cuspids, and eight molars.
The tooth eruption chart (Box 1.9) lists both baby teeth and permanent teeth (a.k.a. secondary teeth), as well as the average time of eruption and shedding. Variables that may influence the time of tooth eruption include genetics, culture, gender, weight/growth, socioeconomic status, presence of systemic disease, or presence of a syndrome. Typically, the lower central incisors (bottom, middle teeth) are the first to erupt. Sometime around 8 months of age, infants will begin to have opposing teeth (both upper and lower central incisors). With the exception of the molars, primary teeth are typically in place by 2 years of age. Over the next decade, children will shed their primary teeth. Meanwhile, their permanent teeth will erupt. When baby teeth and permanent teeth are both visible in the mouth, a child is said to have mixed dentition.
Clinical Note
Mastication may be altered when teeth are diseased or missing.
Clinical Note
Significant deviation from the average time of tooth eruption alerts a clinician to possible oral issues that may result in changes in the development of functional oral activities. This may require follow-up by a dentist or craniofacial specialist.
Once all the primary teeth have fallen out and all the permanent molars have erupted, the typical adult will have the full complement of 32 permanent teeth—4 central incisors, 4 lateral incisors, 4 cuspids, 8 premolars, 12 molars. Upper teeth are referred to as maxillary dentition; lower teeth are mandibular dentition. While the intent is to keep your permanent teeth throughout your lifetime, some adults may lose some or all teeth. When all teeth are missing, the individual is said to be edentulous. Partial or full dentures may be used in place of missing teeth.
Box 1.9 Tooth Eruption Chart
Clinical Note
Rarely do opposing teeth result in the infant biting the nursing mother (either by accident, or on purpose if they enjoy the reaction). While some mothers choose to stop breastfeeding due to biting, most infants with opposing teeth can learn to breast feed without hurting the mother.
Clinical Note
Speech-language pathologists do not need to know teeth numbering. However, the knowledge is useful when reading reports from other health professionals.
Box 1.10 Universal teeth numbering system for permanent teeth

Box 1.11 Universal teeth numbering system for primary teeth.
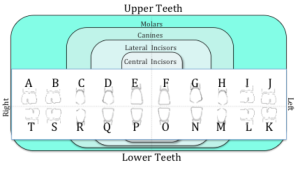
For purposes of labeling and communication, dentists and other professionals concerned with the oral cavity use number or letter systems to identify the teeth. In the commonly used Universal Number System (Boxes 1.10 & 1.11), teeth are labeled in order. Specifically, the adult permanent teeth are divided into 4 quadrants with 8 teeth per quadrant. The upper right quadrant (starting from back) is numbered from 1-8 and then continues around to the upper left from 9-16. Thus, the upper central incisors are numbered 8 and 9. The number system then goes to the lower left with teeth 17 through 24 and continues around to the lower right with 25 to 32. The lower central incisors are 24 and 25.
In the universal number system, primary teeth are labeled with letters starting in the back of the upper right quadrant with A to E, and then F to J on the upper left quadrant; the upper central incisors are E and F (Box 1.11). The labeling system then goes to the lower left in the back and goes from K to O, and continues around to the right with P through T. The lower central incisors are P and O.
Teeth play an obvious role in swallowing, which primarily includes the grinding and mastication of food.
Tongue

The tongue is an important structure in swallowing. It aids in bolus development and bolus control. Additionally, the tongue compresses the bolus providing essential pressure to traverse the oral cavity. Further, as the bolus flow goes from horizontal to vertical, the tongue base applies pressure on the tail of the bolus to aid in its vertical trajectory through the pharynx.
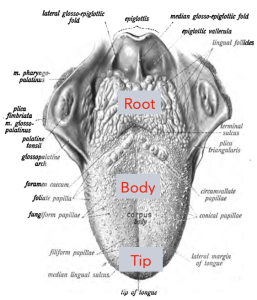
Functionally, we divide the tongue into three parts—(1) back of the tongue (a.k.a. root or base of tongue), which is the part you cannot see when you look in the oral cavity, yet it is essential for a healthy swallow, (2) the blade or main body of the tongue, and (3) the tongue tip (Box 1.12). Collectively the tongue body and tip are important for manipulating food in the mouth—positioning it for mastication and, upon completion of bolus development, positioning it for transport into the pharynx. The tongue base provides final compression on the tail of the bolus as it moves into the pharyngeal cavity.
Box 1.12 Tongue anatomy
The tongue, a muscular hydrostat, lacks a supporting skeletal structure (Kier & Smith, 1985). While the tongue base in the pharynx is muscularly anchored to the hyoid bone via the hyoglossus muscle and some fibers from the genioglossus muscle, the oral tongue is free of skeletal attachment. The inferior tongue is loosely anchored to the floor of mouth via the genioglossus muscle, as well as a tissue band called the lingual frenulum. As a result of this configuration, the oral tongue has significant freedom of movement. However, because the tongue is a muscular hydrostat, it maintains a constant volume. If you protrude the tongue (i.e., stick it out and make it longer), then it becomes thinner to maintain a constant volume. Similarly, if you retract the tongue (make it shorter), then it becomes fatter.
“Want more?”
Historically, if a lingual frenulum was judged to be short, thereby anchoring the tongue in the anterior mouth (referred to

as ankyloglossia or tongue-tie), the frenulum was cut to provide greater degrees of freedom. Today this procedure is reserved for instances when the anchoring impacts feeding.
The tongue surface is covered with papillae (little bumps of various shapes). In Box 1.13, a blue drink temporarily alters the color of the tongue surface illuminating the papillae. These papillae are related to the function of taste. (Note: The tongue is not the only structure that contains taste receptors. This will be discussed in more detail in the section on taste.) Individual taste receptor cells are responsive to one taste; that is, they depolarize in response to a specific chemical ion signature. Thus far, taste buds have been identified that respond to sweet, salty, bitter, acid (sour), or umami (glutamate) tastes. These five taste categories are represented across all areas of the tongue.
Box 1.13 Tongue surface after blue drink.

Just for Fun
Just for Fun
Look in the mirror and inspect the surface of your tongue. Note that there are lots of little bumps distributed on the surface. Observe bigger circular bumps toward the back of tongue body that form a V-shape. To improve visualization, drink a blue slushy and then look again. Also, check out the bumps on the tongues of your family and friends.
Clinical Note


Leukoplakia
When viewing the tongue, you may note oral thrush or oral candidiasis, particularly in patients that are using inhaled or oral steroids, are undergoing radiation treatment, or have suppressed immune systems. When observed, you may note milky white patches distributed throughout the oral cavity, not just on the tongue. The client may also complain of pain in the oral cavity. This should not be confused with oral leukoplakia, which also presents as white patches, but unlike thrush, these patches are “stuck” to the mucosa of the tongue and cannot be brushed away. Patients with leukoplakia usually do not complain of pain and typically have a tobacco history (either smoking or chewing)
On a healthy tongue, the papillae yield a mildly rough surface. A completely smooth tongue surface is usually the result of trauma (e.g., burn) or long-term denture use. Conversely, the tongue surface may have excessive pitting or grooves, or a combination of smooth and rough patches. These surface variants are typically considered normal. However, sometimes they are indicative of, or related to disease. Varying degrees of geographic tongue (varying smooth and rough patches) can change in appearance and is sometimes referred to as benign migratory glossitis. Some individuals with geographic tongue report sensitivity to spice or various tastes. Tongue surface variants may also be related to Down’s syndrome, Sjogren’s syndrome, or psoriasis. Geographic tongue may occur in combination with fissured tongue (deep grooves) (Box 1.14). The incidence of fissured tongue increases with age. When fissured tongue is observed, differential diagnostic consideration should be given to Melkersson-Rosenthanl Syndrome, which is a rare neurological syndrome that has not only fissured tongue, but also facial swelling and paralysis. The prevalence of geographic tongue and/or fissured tongue has been reported in up to 3% in the general healthy population (Shulman & Carpenter, 2006). There is a higher incidence of fissured tongue in individuals with Down’s syndrome.
In addition to tongue surface, oral inspection may reveal shape variations particularly along the lateral border of the healthy tongue (Box 1.14). Scallop marks, when present, may be indentations from the teeth. They may indicate a narrow or small mouth, or a forward carriage of the tongue, as is the case in a tongue thrust. During visual inspection of the oral tongue it is important to note any of the variations discussed above.
Box 1.14 Tongue surface and shape variants
 |
 |
| Fissured tongue | Scalloped tongue |
Clinical Note
Patients with deep fissures should be encouraged to use good oral care, including tongue brushing, to avoid bacteria build up in the fissures.
“Want more?”
There are some vitamin deficiencies that will alter the tongue surface. Iron and folate deficiencies have been linked to a smooth tongue surface
Clinical Note
- Unilateral cortical damage (such as a stroke) may not alter tongue carriage. However, when unilateral asymmetry is noted during tongue protrusion in individuals who have suffered from a cortical stroke, it is likely that in addition to the asymmetry, there is bilateral weakness throughout the tongue.
- In the case of damage to the hypoglossal nerve, motor asymmetry will be noted on the same side as the lesion.
- If on protrusion, the tongue deviates to one side, there is either hypoglossal nerve injury on the side of the tongue deviation, or a cortical lesion on the contralateral side. When noted, inspect the tongue for unilateral atrophy. An individual who recently suffered from a stroke is unlikely to present with unilateral tongue atrophy. Atrophy is often noted with hypoglossal nerve injury (Blondin, Huttner, & Baehring, 2011).
Sensory afferents in the tongue respond to chemical (i.e.,taste) and mechanical stimulus. Sensory input of the tongue is mediated by CN V on the anterior 2/3 of the tongue (the part of the tongue anterior to the tonsil) and CN IX on the posterior third of the tongue. Taste reception is innervated by CN VII in the anterior tongue and CN IX in the posterior tongue.
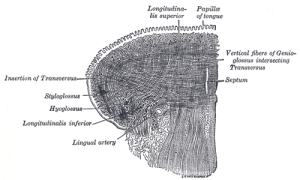
Tongue Muscles
Muscles of the tongue are divided into intrinsic and extrinsic tongue muscles. The intrinsic tongue muscles include the transverse, longitudinal, and vertical muscles (Box 1.15). Although presented individually in this text, the intrinsic tongue muscles work together to change the shape of the tongue. The transverse muscle is fan-like and goes from the center of the tongue to the lateral tongue. When this muscle is contracted the action narrows and elongates the tongue. The superior and inferior longitudinal muscles are long muscles in the medial portion of the tongue. When contracted the result is tongue shortening; if differential contraction is applied to the two layers of longitudinal muscles you can achieve convex and concave structures. The vertical tongue muscle contains small up and down fibers (from bottom to top near tongue surface) that, when contracted, serve to flatten (thin and therefore widen) the tongue.
Box 1.15 Coronal section of tongue showing intrinsic tongue muscles
Public Domain
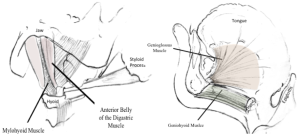
The extrinsic tongue muscles of interest for swallowing include the geniohyoid, genioglossus, hyoglossus, the styloglossus, and the palatoglossus muscles (Box 1.16). Because of the external connections, these muscles can alter the position of the tongue. The genioglossus muscle, which courses from the mandible and then fans out to the inferior surface (i.e., underside) of the tongue, can protrude the tongue or afford anterior carriage of the tongue. The hyoglossus muscle goes from the hyoid bone to the posterior and lateral tongue. Upon contraction this muscle elevates the larynx and depresses the posterior tongue. The styloglossus muscle courses from the styloid process of the temporal bone to the lateral tongue. Contraction of this muscle draws the tongue up and back (retraction); it serves as an antagonist to the genioglossus muscle. The geniohyoid muscle, which courses from the mandible to the hyoid bone, can afford anterior carriage of the hyoid and tongue when swallowing. The geniohyoid muscle serves as an extrinsic tongue muscle, as well as a muscle of the floor of the mouth, and influences the stability of the oral tongue body. The palatoglossus muscle, as mentioned in the section on velar movement, pulls the back of the tongue up when contracted.
Box 1.16 Image Gallery: Extrinsic tongue muscles
Almost all of the intrinsic and extrinsic tongue muscles receive bilateral motor innervation from CN XII. However, the genioglossus muscle receives input from the contralateral cortex only. Moreover, there are two exceptions to CN XII innervation: (1) the palatoglossus muscle is innervated by the pharyngeal branch of CN X and (2) the geniohyoid muscle is innervated by cervical spinal nerve 1 (C1).
Faucial Pillars
In the posterior oral cavity there are two sets of vertical folds of tissue known as the faucial pillars (Box 1.17). The anterior faucial pillars, also known as the palatoglossal arch, houses the palatoglossal muscle and runs from the soft palate to the tongue. This muscle receives motor innervation from CN X. Contraction of this muscle will approximate the soft palate and the base of tongue. The amount of movement of either structure will depend on the stabilization of these structures; the structure that is more stabilized will pull the other structure toward it.
Box 1.17. Faucial pillars
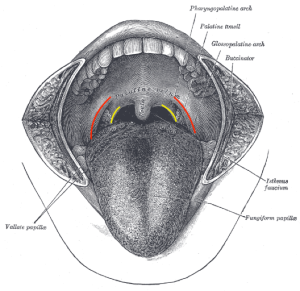
The red line highlights the anterior faucial pillar (palatoglossal fold) and the yellow highlights the posterior faucial pillar (palatopharyngeal fold).
Clinical Note
Although there is much variability in the trigger site, in young healthy adults, the faucial pillar region may be a primary input site for triggering the swallow pattern generator.
Clinical Note
Take careful notice of the anterior and posterior faucial pillars. With intact anatomy, the tonsils are located between these pillars.
Clinical Note
Faucial pillars are targeted in sensory enhancement therapy such as thermal-tactile stimulation.
The posterior faucial pillar, also known as the patalopharyngeal fold, houses the palatopharyngeal muscle and goes from the soft palate to the pharynx. This muscle receives motor innervation from CN X. Contraction of this muscle will shorten the pharynx, thereby shortening the bolus’ journey through the pharynx. In some individuals, appropriate stimulation of the faucial pillar region has been linked to timely trigger of the pharyngeal swallow.
Jaw
The upper and lower jaw bones are the largest facial bones. The lower bone is referred to as the mandible (Box 1.18); the upper bone is the maxilla. (See Box 1.19 for various images of jaw bone and muscles.) The maxilla, although typically referred to as one bone, is a pair of fused pyramidal-shaped bones. The inferior aspect of the maxilla houses the upper teeth. Of importance to swallowing is the horizontal process on the lingual side of the bone known as the palatine process. This process projects medially and sutures at midline to form the hard palate.
Box 1.18 Video
Mandible
Box 1.19 Image Gallery: Jaw bones and muscles
(CC BY 4.0 Download for free at http://cnx.org/contents/ff1ab679-4c9d-4b8f-9792-6da5fdba00d3@3
Clinical Note
Damage to any aspect of the jaw (bones or muscles) will impact mastication and bolus manipulation.
The mandible (lower jaw bone) is a horizontally-oriented, U-shaped bone with anteriorly directed projections on the posterior aspects of the U. The midpoint of the bone (at the chin) is referred to as the mental symphysis or genium. The posterior aspect where the bone bends is referred to as the angle; the upward projection is called the ramus of the mandible. The mandible provides one of the bony attachments for the tongue (via extrinsic tongue muscles). It also provides bony attachment via floor-of-mouth muscles to the hyolaryngeal complex, an important linkage for swallowing. This interesting architecture allows the muscles to do one of two different movements depending on the point of stabilization. If stabilization comes from the mandible, muscle contraction will pull the hyolaryngeal complex toward the jaw. If the stabilization comes from below the larynx, then the contraction of the muscles attached to the mandible will result in opening the jaw (lowering the mandible), pulling it closer to the hyolaryngeal complex. Simply stated, this configuration allows the hyoid to move up or the mandible to move down.
The movement of the mandible is a function of the temporomandibular joint (TMJ), a synovial joint between the mandible bone and the temporal bone. The joint configuration allows for movement that is rotational and translational. In simple terms, the mandible can move down while rotating back and move up while rotating forward. It can also move side to side.
Jaw Muscles
The mandible and maxilla serve as insertion points for jaw muscles (Box 1.19). Jaw muscles can be divided into those that aid in opening the jaw (i.e., jaw opening or depressor muscles) or closing the jaw (i.e., jaw closing or elevator muscles). The primary muscles of jaw opening include the geniohyoid, anterior belly of the digastric (ABD), and the lateral pterygoid muscles. Jaw opening is further assisted by turning off jaw-closing muscles, as well as gravity when an individual is in an upright position. The geniohyoid muscle courses from the genium of the mandible to the hyoid bone. The digastric muscle is composed of 2 bellies–anterior and posterior. ABD courses from the genium of the mandible on either side of the midline to the hyoid bone. The posterior belly continues to the mastoid process of the temporal bone. The lateral pterygoid muscle courses from the sphenoid bone to the temporomandibular joint. Upon contraction these muscles may open, protrude, or lateralize the jaw from side to side. The ABD and lateral pterygoid muscles receive motor innervation from the mandibular branch of CN V. The geniohyoid muscle receives its innervation from C1.
Box 1.20 Floor of mouth muscles
Muscles that elevate or close the jaw include the temporalis, masseter, and medial pterygoid muscles. The temporalis muscle courses from the temporal fossa and fans across the temporal bone. The masseter muscle is a large muscle that goes from the zygomatic arch to the ramus of the mandible. The medial pterygoid muscle goes from the lateral pterygoid plate to the ramus of the mandible. Collectively, these muscles close or elevate the jaw. All jaw-closing muscles are innervated by the mandibular branch of CN V.
Cortical input to CN V comes from both hemispheres, which means that the upper motor neuron inputs that go to the trigeminal motor nucleus come from both sides of the cortex. The trigeminal motor nucleus innervates all the jaw muscles except for geniohyoid. Thus, in unilateral cortical damage, the trigeminal motor unit will still be supported by the opposite side of the brain. Generalized weakness with symmetrical movement in the jaw implies a cortical deficit. If asymmetrical tracking is observed during jaw closing, suspect damage at the level of the trigeminal motor nucleus or the downstream part of the trigeminal nerve.
Jaw bones and muscles are essential in the process of mastication. Chewing typically engages all the range of motion of the mandible by using an up and down/rotary action. Damage to any of the jaw structure or muscles may impact chewing and swallow function.
Floor of Mouth
The floor of the mouth is composed primarily of the geniohyoid and mylohyoid muscles (Box 1.20). The ABD and genioglossus muscles are also considered part of the floor of the mouth complex. The geniohyoid muscle courses from the genium of the mandible to the hyoid bone. The fibers of the mylohyoid muscle fan across the mandible and insert onto the hyoid bone. The ABD muscle goes from the lower border of the mandible just lateral of the mental symphysis to the hyoid bone. The genioglossus muscle courses from the mental symphysis of the mandible to the under surface of the tongue.
“Want more?”
Learn more about floor of mouth anatomy by reading La’Porte, Juttla, and Lingam (2011).
Clinical Note
Oral weakness or poor bolus control can result in material being pocketed in the oral spaces putting the patient at risk for aspiration after the swallow.
For these muscles, the result of muscle contraction is dependent on the point of stabilization. If the jaw is stabilized, then contraction of any of these muscles will pull the hyoid (and therefore the larynx) in a superior and anterior trajectory (toward the mandible). The mylohyoid is linked to superior movement of the hyo-laryngeal complex; the geniohyoid is linked more to anterior movement (Pearson, Langmore, & Zumwalt, 2011). If the hyoid is stabilized from below, then contraction of any of these muscles will assist in jaw opening. For swallowing, the FOM muscles are essential to aid in upward hyo-laryngeal trajectory. The mandibular branch of CN V innervates the mylohyoid and ABD. Geniohyoid is innervated by C1; the genioglossus muscle is innervated by CN XII.
Oral Spaces
The juxtaposition of the oral structures results in oral spaces (Box 1.21). During swallowing, spaces can serve as passageways or resting spots for the bolus. Thus, it is important to review the oropharyngeal spaces with respect to swallowing. Oral spaces of importance include the anterior sulcus (space between the teeth and lip), lateral sulcus (space between the teeth and cheek), and floor of mouth (under the tongue).
Box 1.21. Oral spaces