Rehabilitative Treatment
Rehabilitative approaches used to treat dysphagia seek to restore the function of the subsystems of swallowing resulting in a long-term change to the swallow physiology. Rehabilitative techniques should result in a change in muscle physiology (peripheral changes) and/or neural adaption (central changes). Rehabilitative strategies may be direct, which means that they include swallowing of specific boluses in a controlled condition, or indirect, which means that oral intake is not included as part of the exercise. Ideally, rehabilitative treatment approaches allow for the elimination of compensatory strategies. Over time, with repetition, rehabilitative techniques, which may include strength training, skill training, or training of timing and coordination, should restore aspects of swallow function.
Strength Training
Swallow is a pressure-driven event that is influenced by the strength of the swallow. When weakness occurs, improvements may be achieved through strength training. Before designing and initiating a strength training program to improve swallow function, clinicians must be aware of the principles of strength training to obtain the maximal effect from the rehabilitative program. Aspects of strength training include the type of muscle fiber and muscle configuration being trained, the task being trained, and the training protocol including progressive resistance, intensity, and frequency of the strengthening protocol. Strength training is achieved through structured exercise. General activity is not the same as exercise, although it is certainly better than inactivity. The goal of strength training is long-term improvement of swallow physiology. Thus, strength training should be geared to increase force or pressure, or improve power, timing and/or endurance of muscles involved in swallowing and resulting swallow events.
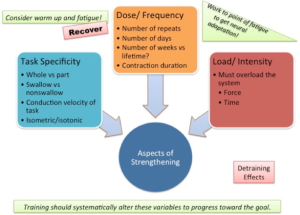
In this section we will discuss common principles for strength training and their application to oropharyngeal muscles. Strength training should systematically alter and control each of these variables to progress towards a goal.
Muscle Fiber Types
Recall the divisions of muscle fiber types and their force generation profile (Box 4.26). Although muscles may contain multiple fiber types, there tends to be a predominance of a fiber type within a muscle compartment. Grossly, skeletal muscle can be divided into 3 fiber types, commonly referred to as Type I, which are slow twitch, fatigue-resistant fibers, Type IIa, which are fast twitch fibers that are somewhat fatigue-resistant, and Type IIb, which are fast twitch fibers that are highly fatiguable. Muscles composed of a predominance of Type II fibers are better suited for quick forceful movements, whereas muscles with predominately Type I fibers are better suited for low force, high endurance activities. It is assumed that much of swallowing is dependent on the function of Type II fibers.
Box 4.26: Muscle fiber types

Fiber type is not static. With injury or changes in muscle activity, fiber types can change. For example, in a healthy individual, sprinting can lead to increases in Type II fibers, whereas distance running can lead to increases in Type 1 fibers. With long term deconditioning, which may occur due to injury or medical event, there is a tendency for muscle fibers to shift to Type II fibers. Further, Type II fibers are more susceptible to deconditioning. This translates to higher fatiguability in our patient population. This deconditioning can be further impacted in individuals over the age of 50 when the effects of sarcopenia (age-related loss of muscle use) may begin to occur.
Clinical Note
Tongue tip is predominantly composed of Type I fibers ,which is supportive of mastication across a mealtime or long periods of articulating. The tongue base is predominantly Type II fibers, which is supportive of the quick and forceful pressure generation during tongue base retraction needed for efficient swallowing.
Terminology
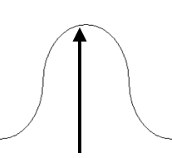
In our field, the terms that are commonly used to describe muscle function include force or pressure, power, speed, and endurance (Box 4.27). Although technically different, in the SLP literature, the terms force and pressure are sometimes used interchangeably.
Box 4.27: Terminology

In muscle physiology, measures of pressure and force are used to reflect strength. Muscle strength is measured when you place a force against a resistance. These measurements can be done during functional activities, such as swallowing, or isolated maximal strength abilities, such as pressing your tongue as hard as you can against your palate. Functional reserve is the difference between maximal strength generation and the strength required for a functional activity. A muscle or system is considered weak when it has a reduced ability to produce force, which may impact functional force generation, range of motion, or speed of movement.
Clinical Note
Sarcopenia (age-related loss in muscle mass) is highly correlated with level of activity lending support to the old adage, “use it or lose it”. Effects of sarcopenia have been reported as early as age 50 and increase with advanced age. Effects of sarcopenia can be reduced with exercise.
Power denotes the strength as a function of time to peak output. In essence, power refers to the speed at which a muscle can produce a desired force (conduction velocity). One can increase power by producing greater force, while maintaining the rate of contraction, or by increasing the contraction speed, while holding a constant force.
Endurance is the duration of time that an individual can produce a given force, typically sub-maximal, against a resistance. Endurance is important in mealtime as activities, such as mastication, are repeated throughout the entire meal.
Muscle strengthening exercises can be isotonic, isometric or isokinetic. Isometric exercise is achieved by generating a forceful contraction without changing the length of the muscle. For example, in a tongue-to-palate press, the tongue increases force generation without changing muscle length. When exercise engages movement that shortens or lengthens a muscle, it is considered an isotonic contraction. Lifting a heavy suitcase from the floor to the table will require an isotonic contraction. Isokinetic refers to a repetitive muscular activity produced at a constant speed, such as cycling on a stationary bike. A pulsed chin tuck against a constant resistance is isokinetic.
Use it or Lose it
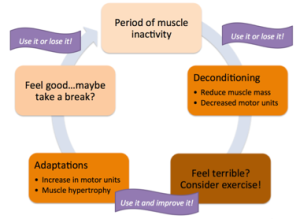
The Use It or Lose It principle has been well discussed in the exercise science literature (Box 4.28). Simply stated, when you discontinue a form of muscle activity, those muscles will fall victim to disuse atrophy. Further, the specialized skills for a particular task will decay. Fortunately this principle partners with another—Use It and Improve It. That is, if the given system has not been used for a period of time resulting in loss of function or skill, reuse of the system will restore strength and skill. Because we eat and swallow every day as part of our daily routine, swallow skills are typically not a victim of disuse atrophy in healthy individuals with a normal diet of varied textures and consistencies. However, when swallow function becomes impaired or if oral intake is halted for medical reasons, deconditioning of the swallow muscles may occur. If this disuse is lengthy, deficits should be anticipated and training may be required to regain function. In special cases, for example, elderly or edentulous individuals who change their eating habits to a more restricted diet, swallow capabilities may degrade as a result of the diminished muscle requirements for their daily intake.
Box 4.28: Cycle of muscle inactivity
Task Specificity & Transference
Task specificity is an important variable in strength training. Ideally, when trying to improve a specific task, training should closely mimic that task. In general, strength training is best performed as a highly integrated WHOLE task for it to best impact neural pathways. Thus, the best exercise to improve swallowing is to swallow. Unfortunately, in dysphagia management swallowing may not always be possible.
When swallows cannot be safely incorporated into the daily routine or treatment protocol, aspects of the required task can be enhanced and later transferred to the functional task. In transference, you use a piece of a task and train that piece to improve the overall function. In this case, instead of swallowing, the treatment focus is placed on one aspect of the swallow. For example, lip strength can be improved to help reduce anterior spillage; tongue strength can be increased to improve swallow pressures or oral bolus manipulation. Non-swallow exercises are useful for patients who are required to maintain a non-oral status, or are not yet safe for oral intake. For some patients, particularly those with cognitive deficits, smaller tasks are easier to achieve. Non-swallow tasks may allow for better control of intensity and other dosing parameters (Box 4.29).
Box 4.29: A schematic reflecting parameters that can alter the outcome of strength training
Motor Learning
When teaching a new task or reconditioning an old task (undoing a learned pattern that may be inefficient) consider the stages of motor learning. In the beginning, learning is largely cognitive and focuses on understanding the desired motor pattern and visualizing the completion of the task. This is followed by practice performing and correctly completing the motor task. During this stage, cues and guidance are provided at a decreasing rate until the individual can perform the task independently. This stage is further supported by reflection on performance. Repetition of the correct motor pattern leads to the final stage where the motor pattern can be automatically produced in the right context without therapeutic guidance of specific cognitive focus. As an example, consider a patient who has late onset glottal closure during the swallow. A new pattern of timing is introduced and practiced until automated.
Intensity
Intensity is the resistance to movement or the amount of force applied to a given object. To achieve physiologic muscle changes, the muscle must be taxed beyond its typical workload with respect to either force or time (or both) (Trombly, 1983). Intensity can be manipulated by changing the force used during a task, the time used to complete a given number of repeats, or the total time required to perform the task (Box 4.29). The chosen approach to intensity should closely mimic the desired task. Consider if the goal is to increase the swallow strength, speed, or endurance across a mealtime. Endurance can be trained and enhanced through the use of low levels of resistance over extended time; strength can be enhanced with repetitions of high-resistance exercises; power is trained by performing strength tasks with time requirements. If intensity is maintained at near-maximum strength, the greatest changes will be observed in strength, but not endurance. At midrange intensities, strength training also improves endurance. Note that the exercise speeds should closely match the speed of the desired outcome. That means that if you wish your patient to complete an average meal in 45 minutes or less, the practice should incorporate many swallows in a short time period. Rest periods after each swallow may dilute the impact of strength training. For progression toward the ultimate goal, there should be progressive resistance over time to keep a constant intensity as a patient gets stronger. That is, the level of exercise should always be adjusted to accommodate the strengthening system.
Clinical Note
According to the Academy of Sports Medicine, to effect muscular change you should work the system somewhere between 60-80% of maximal strength.
Clinical Note
To increase muscle strength, you must work to a point of fatigue. This is achieved by choosing an appropriate intensity and dose parameters.
Dose Parameters
Treatment dose is related to intensity (Box 4.29). This refers to the frequency that the exercise(s) is being performed. Dose can be broken down into several parameters including the number of repetitions in a set, the number of sets in a session, the number of sessions in a day, and the number of days per week that the regime is performed. For oropharyngeal muscles, there are no clear guidelines and various protocols are used. One example of an exercise protocol is the 5-5-5- protocol. Briefly this means that you perform 5 sets of 5 tasks to complete a session. The session is repeated 5 times a day and this is completed 5 days a week. While this may be adequate for non-swallow transference exercises, it does not reflect the amount of swallows that must be produced in a mealtime. Therefore, if that is the goal, dosing should allow for practice that mimics the needed frequency.
Recovery
Recovery is required to maximize the benefits of strength training. As noted, in order to effect change at the level of the muscle, you must provide overload that is progressive over time. However, when overload is performed without consideration for recovery, injury may occur.
In general, adequate recovery time must be provided between exercise sessions. There are physiologic reasons to provide recovery time. For large muscles, during recovery, the muscle’s glycogen and oxygen stores are replenished, while waste products are removed. Unfortunately, there are no data available regarding typical recovery patterns for the oropharyngeal musculature used during swallowing. There is also no data on the impact of disease on the needed recovery time for these small muscles of swallowing.
Deconditioning
Deconditioning or disuse atrophy occurs with reduction in muscle use and results in a reduced muscle cross-sectional area. In most cases, deconditioning occurs quickly and tends to preferentially affect Type II fibers. This is unfortunate, as it is likely that Type II fibers are more important for swallow function than Type I fibers. Deconditioning can happen for various reasons. With illness and dysphagia there may be a reduction in spontaneous saliva swallows. Further, there may be alterations to diet type with a tendency toward less complex foods. The end result is reduced muscle activity. In addition, those relying on non-oral feeding methods have less opportunity to swallow, which may further exacerbate the deconditioning process.
Sarcopenia is a form of generalized deconditioning, where the muscle loss is considered a normal aspect of aging and likely due to changes in lifestyle and levels of activity. However, there is evidence that sarcopenia can be reduced with programmatic exercise.
Oropharyngeal Strengthening
As swallow is a pressure-driven event, some threshold of oromotor strength and power is required to generate adequate pressure to produce a sufficiently safe and efficient swallow. To confirm the potential for strength training through isometric tongue-to-palate press exercises, Palmer and colleagues (2008) measured muscle activation via EMG of individual muscles during defined levels of pressure (Box 4.30). For various oropharyngeal muscles, namely the geniohyoid, mylohyoid, genioglossus, and medial pterygoid, there is a clear relationship between the muscle activation and force production, supporting the hypothesis that greater muscle activity produces greater pressures (Palmer et al., 2008). Conversely, weak muscles produce less pressure and generate a weaker swallow. It is postulated that by strengthening weak muscles, force generation is improved. Strengthening can be applied to muscle groups associated with a structure, such as tongue or lip, or during a functional task, such as an effortful swallow. Regardless, if a patient has a weak swallow, the ultimate goal is to improve the strength thereby rendering the swallow safer and more efficient.
Box 4.30: Relationship between pressure and muscle activation

Data from Palmer et al., 2008
As discussed earlier, training can be task specific or incorporate a piece of the task in hopes of transference to the swallow. When individual components of the swallow are trained, they may focus on, for example, increasing tongue strength or lip strength.
Clinical Note
If the goal is to improve swallow over a mealtime, then within a treatment session,the goal should be to have a patient perform at least 30 swallows within a treatment session, which can range from 30 to 60 minutes.
Improving strength, power or endurance can be achieved using low-technology resistance devices, such as a tongue depressor or finger press. More sophisticated devices that measure pressure or muscle activation, allow for better control of intensity and dosing parameters, and may also serve as a biofeedback device. Box 4.31 provides a list of parameters to consider when choosing a resistance strengthening device. Box 4.32 provide a summary of available pressure devices.
Box 4.31: Parameters to consider when choosing a device
Is it practical?
- Is it affordable?
- Is it portable?
- Does it require excessive training or certification for use?
- Is it easily available?
- Does it provide quantifiable data?
- Is data extraction and analysis efficient?
Is it flexible?
- Can it be used for training the WHOLE swallow or a swallow-specific skill?
- Can it be adjusted for varying loads?
- Can the resistance be progressively adjusted?
Is there supportive evidence?
- Is there efficacy data using the device?
- What level of evidence is available?
- What patient populations were used in the experimental studies?
Box 4.32: Equipment used for strength, power, and endurance training
|
IOPI |
MOST |
Tongue Press |
|
|
|
 |
 |
 |
|
description |
Air-filled oral sensor connects to a pressure transducer. Portable and digital interface. |
Palate-shaped oral sensor connects to a pressure transducer. Portable and digital interface. |
Portable and cheap water—filled bulb that uses compression to estimate resistance |
|
resistance |
Progressive and Measurable |
Progressive and Measurable |
Gross estimate with limited progression |
| website | http://iopimedical.com | http://www.swallowsolutions.com/product-information/swallowstrong-device | http://www.therasip.com |
Clinical Note
Increasing strength alone may not be sufficient to obtain maximal swallow efficiency. Consider activities or skills that connect the increased strength (or power or endurance) to the aspect of the swallow task that needs attention.
Tongue Strengthening
Patients with severe dysphagia show reduced tongue strength (Palmer et al., 2006). Also, tongue strength decreases with age, and while this strength may be functional for swallowing, in geriatric individuals, it may lead to an increased risk for dysphagia in the presence of other conditions that commonly affect elderly individuals, such as stroke or progressive neurologic conditions. Reduced tongue-to-palate pressure may result in reduced oral bolus control, hyoid elevation, and base of tongue to posterior pharyngeal wall contact (Lazarus et al., 2000; Park, Kim, & Oh, 2015). The ability of the tongue to adequately generate oral pressures may also impact pharyngeal pressure. When weakness is noted, tongue-to-palate pressure can be used as an exercise to increase strength, power, or endurance of the tongue, and aspects of swallow function.
Box 4.33: Sample tongue strengthening protocol using tongue to palate press
- Minimum treatment length is 6 weeks.
- Measure tongue-to-palate max. Use this measure to set the pressure goal for strength training. Set resistance at 75% of the max.
- This is repeated each week to reassess the max and adjust the resistance goal accordingly.
- Push the tongue to the palate until the resistance goal is met and hold for 2 seconds.
- This task is repeated 10 times to make one set.
- A set is performed 5 times throughout the day or during the treatment session
- This is done an average of 5 days a week (and no less than 3 days a week).
Task Specific Modifications:
- Instead of producing a tongue press to palate, produce an effortful swallow.
Clinical Note
Improved tongue strength has been linked to improved pharyngeal transit and base of tongue to posterior pharyngeal wall contact.
Clinical Note
Across a variety of studies and measuring devices maximum isometric strength during a tongue to palate press in healthy adults falls in the range of 50 to 75 kilopascals (kPa). High variability in maximal strength is typical across developing individuals (infant to adult), and in individuals of advanced ages (>70 years old). Generally, with advanced age, there is a decline in maximal strength performance.
Procedure
Historically tongue strength was performed by having a patient press their tongue against a tongue depressor or gloved finger, where the resistance was graded by the clinician. More recently, devices have become available that serve specifically to improve tongue-to-palate pressure profiles. Box 4.32 provides an overview of some available devices. All devices are easily portable, vary in their ability to provide progressive measurable resistance, and can be used to train pressure profiles in the tongue or during swallow specific activities, such as an effortful swallow. Devices can also be used to provide biofeedback.
Although there is limited evidence to provide specific procedural guidelines for the small oropharyngeal muscles, general practices can be drawn from protocols proposed for large muscles by the Academy of Sport Medicine. Using these guidelines, treatment should not be less than 4 weeks and is better with a minimum of 6 weeks. If not contraindicated, at least 70% of maximal strength should be used as a strength target to effect muscular change. As maximal strength increases, so should the desired strength target. Repetitions should be at least 3 sets of 10, and should be done a minimum of 5 days a week. Within a session, which can range from 30 to 60 minutes, task specificity should be addressed; the goal should be to have at least 30 swallows completed during the session.
Efficacy
Tongue strengthening through the use of increasing tongue-to-palate pressure profiles has been studied in healthy individuals, healthy elderly, patients with dysphagia due to stroke (Robbins et al., 2007) and patients with head and neck cancer (Lazarus et al., 2014). While the results from Lazarus and colleagues (2014) did not show an effect on swallowing, in most cases, when honoring principles of strength training, tongue pressure profiles are increased. Further, changes in both oral and pharyngeal swallow function are observed with increased tongue strength. Although limited, the current efficacy supports the use of strength training in some patient populations.
Lip Strength
Lip strength is important for anterior containment of the bolus in the oral preparatory phase of the swallow. Using protocols similar to those designed to increase tongue strength, lip strength can be improved. The IOPI can be used to provide measurable progressive resistance in a lip strengthening protocol. There are limited data available to assess the efficacy of lip strengthening and its impact on anterior containment or other aspects of the swallow.
Tongue Hold Exercise
The tongue hold exercise, sometimes referred to as the Masako maneuver, is postulated to (a) increase recruitment of the glossopharyngeal portion of the superior pharyngeal constrictor muscle, and (b) improve tongue base retraction. The anticipated result is to shorten the pharynx, and improve pharyngeal driving pressure (Fujiu & Logemann, 1996; Umeki et al., 2009; Doeltgen, Witte, Gumbley, & Huckabee, 2009).
This technique was first described by Fujiu & Logemann (1996). When this approach was observed using VFES in patients with oral cancer, they noted increased anterior bulging or movement of the posterior pharyngeal wall which yielded improved tongue base contact to the posterior pharyngeal wall. Despite the fact that this was originally referred to as a maneuver, it is not a compensatory strategy. In fact, this technique increases the risk of aspiration when done with a liquid or food bolus.
The treatment is most appropriate for individuals with reduced or weak base of tongue (BOT) movements. Because this maneuver reduces the anterior motion of the hyoid bone, patients with poor hyo-laryngeal trajectory may not benefit from the use of this technique.
Procedure
Performance of this technique is simple — the tongue is extended past the lips and remains there during a saliva swallow (Box 4.34). If the patient cannot maintain tongue protrusion the tongue may be gently held at the tip. This action is repeated. It is possible that progressive resistance may be achieved by controlling the percent of maximal tongue extension. More specifically, after measuring the maximal tongue protrusion past the teeth, the clinician can have the patient perform the exercise with a designated percentage of maximal tongue protrusion. Across the treatment period, the percent of maximal tongue protrusion can progress under the assumption that greater tongue protrusion leads to greater resistance. However, this assumption has not been well explored in the literature. The technique employs task specificity as the patient is performing an actual swallow, albeit slightly altered, during the exercise. approximates some of the criteria of strength training. When oral dryness occurs, misting the oral cavity can aid in continued use of the technique.
Box 4.34: Sample tongue-hold (Masako) exercise
- Minimum treatment length is not explored in the literature, but it is likely that a minimum of 4 weeks is needed to achieve the desired goal.
- Measure maximal tongue protrusion past the teeth
- This may be repeated each week to note any changes
- There is no literature to support the use of percent of tongue protrusion as progressive resistance
- Choose percent of maximal tongue protrusion for initial treatment and progress tongue protrusion to near max position throughout the course of treatment
- With the tongue protruded, the patient is instructed to swallow.
- Due to increased risk of aspiration, only saliva swallows are used in this exercise
- Treatment dosing parameters are selected and followed through the course of treatment. See the sample tongue strengthening protocol for an example of dosing parameters .
Task Specific Modifications:
- If repeated swallows result in oral dryness, the oral cavity can be misted, or sips of water can be used between sets.
Efficacy
To date, much of the data have explored the impact of the tongue hold exercise on the swallow during the performance of the technique, rather than assessing changes over time and the impact on swallow function. Oh and colleagues explored the efficacy of the Masako in healthy individuals (Oh, Park, Cha, Woo, & Kim, 2012). While the evidence is disappointing, the limitations of the study make it difficult to rule out this exercise. In short, the use of healthy participants may have precluded the authors from identifying any long term effect of this exercise. Given the little evidence of the technique’s efficacy as a rehabilitative exercise, treatment progress should be carefully and repeatedly monitored for its impact on functional swallow. The exercise should be discontinued if no change is noted with respect to the hypothesized parameters – base of tongue to posterior pharyngeal wall contact and swallow driving pressure as noted in changes to pharyngeal transit or reductions in pharyngeal residue.
Shaker Exercise
The Shaker exercise, also referred to as the head-lift or head-raise exercise, was originally designed to strengthen the suprahyoid muscles involved in the elevation of the hyo-laryngeal complex. It has also been proposed as a treatment for age-related dysphagia due to sarcopenia (reduced muscle function associated with age) (Easterling, Grande, Kern, Sears, & Shaker, 2005). Strengthening of these muscles are hypothesized to improve hyo-laryngeal trajectory during the swallow, resulting in a widening of the UES opening yielding improved bolus clearance. The desired outcome of the exercise is to reduce or eliminate aspiration after the swallow (i.e., aspiration of pharyngeal residue).
Procedure
The Shaker exercise protocol contains two exercise activities — isometric and isotonic contractions (Box 4.35). The exercise is performed on a flat surface where the patient lays on their back. In part 1 of the exercise protocol, the patient lifts their head while maintaining shoulder contact to the floor. Sample instructions may include, “While keeping your shoulders on the floor, lift your head and look at your feet.” The head is held in the elevated position for 60 seconds. This task is repeated 3 times with a 1 minute rest period between each trial.
Box 4.35: Shaker exercise protocol
- Recommended treatment length is 6 weeks
- Patient is placed in supine position for both exercises in this protocol
- Exercise 1: Isometric
- Instructions: “Lift your head and look at your feet while keeping your shoulders down. You will do this for 1 minute. I will tell you when to stop.”
- This is held for 60 seconds
- This is performed 3 times with a 1 minute rest between each trial
- Exercise 2: Isotonic
- Instructions: “Lift your head and look at your feet while keeping your shoulders down. Hold for 1 second and release. You will repeat this pulse 30 times. I will count for you.”
- The patient lifts and lowers the head at a rate of 1 lift per second.
- This is performed 30 times
- The combination of these 2 exercises described above serves as 1 set. Three sets are performed daily over the course of treatment.
Protocol Modifications:
- Although the developers do not identify any modifications, many have been used in the clinic including the following.
- For patients with low back issues, feet can be elevated on a chair and patient is provided a gaze point approximate to the desired location.
- For patients who have difficulty disengaging head lift from shoulder lift, the shoulders can be stabilized by the clinician or with the use of sand bags.
- For patients who are unable to achieve a 60 second head lift, performing isometric hold for a reduced amount of time that allows the patient to experience overload of the system can be used. Attempts can be made to structure the exercises so that the patient gradually and systematically progresses to the desired end point.
- Provide verbal encouragement as needed to achieve desired goal.
In part 2 of the exercise protocol, the head is lifted and immediately lowered. This head pulse is performed 30 times at a rate of approximately one lift per second. The patient is encouraged to lift their head to the full range of motion needed to visualize the feet without lifting the shoulders from the surface. Three sets of 30 are performed with 1 minute rest between each trial. The isometric and isokinetic trials combine to make 1 set. The exercise set is performed 3 times a day over the course of a 6 week treatment period.
While the Shaker head lift and head hold exercises have been clearly outlined by the developers, some clinicians employ modifications based on patient ability. Common clinical modifications include (a) performing the head lift to an individual’s maximal time, which may be less than 60 seconds, or (b) stabilizing shoulders with weight such as sand bags or with the hands of the clinician or caregiver. There have also been attempts to perform this in sitting position using resistance, such as elastic bands around the forehead.
To perform this exercise, individuals need to have (a) enough mobility to achieve and maintain the supine position, (b) adequate muscle integrity to perform the task, and (c) adequate cognitive function to complete the exercise without clinician input or supervision. It has been used successfully in healthy elderly individuals who experience sarcopenic-related dysphagia (Easterling et al., 2005), as well as patients post stroke or those being treated for head and neck cancer (Ohba et al., 2016). It has also been shown to aid in transition from tube feeding to oral feeding (Shaker et al., 2002; Logemann et al., 2009). Individuals with degenerative neuromuscular disease, such as myasthenia gravis or muscular dystrophy, or cervical neck problems, such as arthritis or post fixation, may not be appropriate candidates for this protocol.
Efficacy
Level 1 evidence exists to support the use of the Shaker exercise to improve superior and anterior hyo-laryngeal trajectory in healthy elderly and individuals with dysphagia (Shaker et al., 1997; Shaker et al., 2002; Logemann et al., 2009). Yet, the evidence is inconsistent regarding the impact of the improved hyo-laryngeal trajectory to alter UES opening, pyriform sinus residue and airway protection (Shaker et al., 1997; Shaker et al., 2002, Logemann et al., 2009; Gao & Zhang, 2017).
Limitations
Based on evidence from EMG, the Shaker exercise does recruit and fatigue the suprahyoid and infrahyoid musculature, which are essential in hyo-laryngeal trajectory. However, the sternocleidomastoid muscle is also recruited (Ferdjallah, Wertsch, & Shaker, 2000). While the infrahyoid and suprahyoid musculature recover quickly from fatigue, the sternocleidomastoid muscle does not. The primary limitation of this protocol is reduced adherence due to neck pain or soreness. Also, some patients report difficulty with integrating the exercise into their daily routines due to the intense nature of the program.
Chin Tuck Against Resistance
The chin tuck against resistance (CTAR) was originally proposed as an alternative to the Shaker exercise for individuals who were unable to perform the Shaker exercise due to its intensity or an inability to get on the floor, either for reasons of limited mobility or medical issues such as severe reflux. For that reason, the CTAR is sometimes referred to as the modified Shaker exercise. Similar to the Shaker, the CTAR aims to improve the strength of the suprahyoid musculature to effect change in UES opening and reduce pyriform sinus residue. The CTAR contains both isometric and isotonic exercise components. Resistance to the chin tuck action is provided through the use of ball held under the chin, a neck resistance device secured under the chin (such as the isoflex), or resistance band used on the forehead. Of these, the first two are the most commonly employed.
Procedure
The CTAR exercise protocol mimics the Shaker exercise protocol (Box 4.36). Using a resistance (e.g., rubber ball), the patient pushes their chin against it. The action of pushing against the ball with the chin “as hard as possible and release” is repeated 30 times. The same action is performed with a prolonged hold.
Box 4.36: CTAR exercise protocol
- Recommended treatment length is 6 weeks
- Patient is placed in supine position for both exercises in this protocol
- Exercise 1: Isometric
- Instructions: “Lift your head and look at your feet while keeping shoulders down”
- This is held for 60 seconds
- This is performed 3 times with a 1 minute rest between each trial
- Exercise 2: Isotonic
- The patient lifts and lowers the head at a rate of 1 lift per second.
- This is performed 30 times
- The combination of these 2 exercises described above serves as 1 set. Three sets are performed daily over the course of treatment.
Protocol Modifications:
- Although the developers do not identify any modifications, many have been used in the clinic including the following.
- For patients with low back issues, feet can be elevated on a chair and patient is provided a gaze point approximate to the desired location
- For patients who have difficulty disengaging head lift from shoulder lift, the shoulders can be stabilized by the clinician or with the use of sand bags
- For patients who are unable to achieve a 60 second head lift, performing isometric hold for a reduced amount of time that allows the patient to experience overload of the system can be used. Attempts can be made to structure the exercises so that the patient gradually and systematically progresses to the desired end point
While in the original articles, the CTAR used a ball for resistance, other devices can be used. In our lab, we piggy back resistance devices with a pressure transducer (eg, IOPI) so that the chin to chest action can be measured and resistance can be controlled and progressed.
Efficacy
Current literature supports that the CTAR is a good alternative to the Shaker exercise for individuals who are unable to maintain a supine position for an extended period of time. It is important to note that of the currently available efficacy studies, most were performed on healthy individuals. Like the Shaker, the CTAR was sufficient to activate and exercise the suprahyoid muscles (Yoon, Khoo, & Liow, 2014; Sze, Yoon, Escoffier, & Liow, 2016). Unlike Shaker, the CTAR does not engage the sternocleidomastoid, and therefore, the issues of fatigue and neck pain were not reported in the healthy population tested. For a group of patients post stroke with dysphagia, the CTAR did prove as efficacious in improving swallow safety as the Shaker (Gao & Zhang, 2017). Yet, the CTAR resulted in better quality of life.
Velar Valving
Reduced velopharyngeal closure during the swallow results in reduced pressure generation imparted on the bolus and increases the risk of nasopharyngeal reflux. Because nasopharyngeal reflux is associated with sinus disease and pediatric apnea, it is important to identify treatment to help reduce nasopharyngeal invasion.
Although there is limited data on the treatment of velar insufficiency for swallowing, there is evidence in the speech literature that the velum can be strengthened with the use of continuous positive airway pressure (CPAP). More research is warranted to address the usefulness of strengthening the velum and its impact on leakage during the swallow.
Bolus Volume and Viscosity
Graded and progressive changes in bolus volume or viscosity can be used to provide progressive resistance in a task specific swallow activity. While there are no efficacy data to assess the effectiveness of this approach, this hypothesis is supported by the fact that EMG shows increased muscle activation with increased bolus viscosity. Across or within a treatment session, bolus volume or viscosity can be incrementally increased to enhance resistance needed to produce a productive swallow. While this may be useful for a patient with a weak swallow, it maybe contraindicated in patients who also have frank aspiration.
Jaw Opening Exercise
The jaw opening exercise (JOE) is based on the fact that jaw opening engages suprahyoid musculature. The developers hypothesize that repeated jaw opening can serve to strengthen the suprahyoid musculature (Wada et al., 2012). If this assumption is correct, the exercise could lead to improved hyo-laryngeal trajectory and greater UES opening. The end result would be to improve bolus clearance. Box 4.37 summarizes the jaw opening exercise protocol. Currently, there is limited evidence to support or negate this hypothesis. Further research is warranted to clarify the procedure and its efficacy.
Box 4.37: Sample jaw opening exercise (JOE) protocol
- Minimum treatment length is not explored in the literature. The initial study had patients perform the exercise for 4 weeks (Wada et al., 2012).
- Open and Hold Exercise
- Have patient open their mouth to maximal opening and hold for 10 seconds
- This is repeated 4 times with a 10 second rest between each trial
- A set is performed twice daily throughout the course of treatment.
Jaw Strength and Range
Reduced jaw strength and range of motion have been implicated in oral dysphagia, specifically with respect to being able to achieve sufficient oral opening for food entry and chewing.
Oral Opening
Adequate oral opening is required to allow entrance of the bolus into the oral cavity. While there is individual variability, most individuals need at least 30 mm of opening to have ease in food entry. For some patients, particularly those that are post surgical or post radiation, trismus or reduced jaw opening may occur. Therapeutic increases in oral opening have been achieved using (a) the jaw opening exercise with manual assist, (b) progressively stacked tongue blades, or (c) a passive jaw opening device, such as the therabite (Box 4.38). Box 4.39 provides a sample protocol to increase oral opening using a passive jaw opening device.
Box 4.38: Therabite jaw motion device

Box 4.39: Sample oral opening exercise protocol with a passive jaw opening device
- Minimum treatment length is not explored in the literature. The primary clinical trial had patients perform the exercise for 4 weeks (Maloney et al., 2002).
- Using the oral opening range of motion scale, determine current oral opening for baseline data.
- Set the device for exercise
-
- With bite pads in place, carefully insert the mouthpiece onto the teeth
- Have patient squeeze down on the device to their maximal opening without discomfort.
- Set the opening by turning the knob on the back of the device.
- This setting should be adjusted as oral opening improves.
- Begin the exercise protocol
-
- Press and hold the device for 7 seconds.
- This is repeated 7 times to make a set.
- Each set is repeated throughout the day 7 times
Comparisons of the efficacy of tongue blades versus a passive jaw motion device show that, in general, both are better than no therapy. However, the passive jaw device results in greater oral opening and reductions in jaw pain when compared to tongue blades (Maloney et al., 2002; Buchbinder, Currivan, Kaplan, & Urken , 1993).
Clinical Note
Medicare and other funding agencies are not inclined to pay for treatment of oral motor opening alone unless the limited jaw opening has functional consequences, such as requiring tube feeding due to inadequate oral opening.
Jaw Strength
Jaw strength may be linked to an individual’s ability to chew and prepare food for safe transit through the pharynx. Typically, in a jaw strengthening protocol, jaw closing muscles are targeted. Resistance can be provided by using a task specific activity with varying bolus complexity. It can also be provided by a jaw motion device that provides resistance to closing. To achieve this, the therabite can be modified with resistance bands placed on the arms of the device. Resistance can be graded by changing the location of the bands with respect to the fulcrum. When no device is available, elastic bands can be placed around the head and under the chin such that oral opening is met with resistance. Although anecdotal evidence is available, there is limited experimental data exploring the efficacy of the therabite with resistance bands or other approaches to improve jaw strength and thereby improve mastication.
Effortful Pitch Glide
The effortful pitch glide is an indirect, non-swallow exercise that combines falsetto voice production with the pharyngeal squeeze maneuvers in hopes of improving hyo-laryngeal elevation and pharyngeal strength. Separately, these aspects mimic biomechanical movements needed in swallowing (Miloro, Pearson, & Langmore, 2014). Specifically, the pitch glide to falsetto engages hyo-laryngeal elevation, whereas the pharyngeal squeeze maneuver engages pharyngeal compression and shortening. This exercise may be useful for improving pharyngeal muscle strength.
The procedure requires the patient to gradually phonate from modal register to their highest falsetto pitch on a prolonged production of /i/. Effort is added at the highest pitch production with a more forceful /i/. The clinician can aid performance by modeling. A FEES scope can be used to show changes in the pharynx as a result of the exercise to aid in training the exercise or provide biofeedback.
There are currently no data available to support or negate the use of this technique. Applying principles of exercise science gives some support as the actions transfer to swallow physiology. The exercise is lacking in clear guidance to provide measurable progressive resistance, or the needed intensity to effect change at the muscular level. That said, if visualization through FEES supports a positive effect of the exercise (i.e., increased pharyngeal compression), this exercise may be appropriate for those individuals.
Lee Silverman Voice Training
Lee Silverman Voice Treatment (LSVT) was originally designed to improve volume and intelligibility in patients with Parkinson’s disease. It has been observed that this treatment has an additional benefit of improving swallow function and swallow-related quality of life (Sharkawi et al., 2002; Palmer, Wohlert, & Easley, 2004). Although evidence is quite limited, preliminary data suggests that there is a direct effect of LSVT on swallow function. After LSVT, some individual have improved oral tongue function for bolus control and improved tongue base retraction. Is also postulated that LSVT may improve glottal valving. If these hypotheses bear out in future research, then LSVT can be employed for individual who have a weak voice and a weak swallow.
Compensatory Strategies as Rehabilitative Treatment
Compensatory maneuvers transiently manipulate swallow physiology through the use of a specific strategy. However, over time consistent use of some maneuvers may result in a long-term alteration to swallow function. Identifying a treatment that serves both a compensatory and rehabilitative function is particularly useful when patients have limited attention or cognitive skills.
Mendelsohn
The Mendelsohn maneuver employs purposeful and prolonged laryngeal elevation during the pharyngeal swallow through voluntary active engagement of suprahyoid musculature. Continued and purposeful use of this activity may strengthen suprahyoid muscles and improve swallow function long term. Explorations of the Mendelssohn as a rehabilitative approach to swallowing were explored in patients post stoke (McCullough et al., 2012; McCullough & Kim, 2013). After two weeks of a Mendelssohn exercise protocol, there were some modest gains in anterior hyoid trajectory and UES opening duration. Patient reported outcomes also improved. While promising, this is a rather limited data set. More research is needed to continue to define the dosing parameters that allow the Mendelsohn to serve as an effective rehabilitative approach.
Effortful Swallow
The effortful swallow encourages voluntary effort that exceeds the usual effort imposed on a bolus. Although established as a compensatory strategy to improve bolus driving pressure, there is evidence that the effortful swallow serves as a task-specific isometric exercise and over time may improve motor function (Huckabee et al., 2005; Wheeler-Hegland, Rosenbek, & Sapeinza., 2008; Clark & Shelton, 2014). The use of the effortful swallow as a rehabilitative approach has not been standardized. However, keeping in line with principles of strength training, it is likely that success will be dependent on the number of trials and the level of effort. Box 4.40 provides a sample of the treatment protocol when using effortful swallow as a rehabilitative exercise. In this scenario, effortful swallow should be practiced in the clinic and at home as an exercise, not only as a adjunct to mealtimes.
Box 4.40: Sample effortful swallow protocol
- Minimum treatment length is not explored in the literature, but it is likely that a minimum of 4 weeks is needed to achieve the desired goal.
- Measure maximal tongue to pressure (use of IOPI or MOST)
- Measure swallow pressure. An effortful swallow should increase the percent of maximal pressure applied during the swallow.
- E.g., If maximal tongue-to-palate pressure is 30kPa, and swallow pressure is 10 kPa, then the goal is to use greater than 30% of the max pressure during swallow.
Neuromuscular Electrical Stimulation
Electrical stimulation, is not a treatment, but rather a modality that can be used to augment muscle strengthening protocols. While there are various types of electrical stimulation (Box 4.41), SLPs use neuromuscular electrical stimulation (NMES) as part of their rehabilitative treatment of dysphagia. Simply, NMES is achieved by pairing a functional swallow activity with a stimulus sufficient enough to result in a neural reaction (i.e., a muscle contraction). Note that the stimulated muscle contraction is not an exact replica of a non-stimulated muscle contraction. However, when the stimulation is coupled with a functional activity, the muscle pattern more closely approximates reality.
Box 4.41: Types of electrical stimulation
- TENS: Used to treat pain
- Iontophoresis used to increase penetration of topical medication
- High Voltage/Pulsed e-stim used to promote wound healing
- NMES used for muscle reeducation or disuse atrophy
NMES uses a stimulator and an electrode to provide electrical stimulation to a muscle or group of muscles. While electrodes can be intramuscular or surface, traditionally surface electrodes are used in swallow treatment. For ease in set up, pre-gelled bipolar electrodes can be purchased. Electrode placement dictates the muscles that will be recruited during the stimulation. For swallowing, often the suprahyoid muscles are of interest and can be recruited through the submental surface.
Clinical Note
Typically, graduate students in speech pathology,receive limited to no training in the use of electrical stimulation as a treatment modality. Therefore, post-graduate certification programs are offered to provide training associated with a specific electrical stimulator.
Limitations and Contraindications
When choosing NMES to augment strength training, it is important to be aware of the limitations and contraindications. NMES should never be delivered over an open wound, a developing fetus, or a pacemaker. Although the dysphagia clinician does not place electrodes near the belly or heart, for safety, medical physician approval should be obtained when considering NMES in individuals who are pregnant or who have a pacemaker. Electrode placement should also avoid the carotid sinus, which is located on the lateral neck. Caution should be used in patients with neurodegenerative disease where strong muscle contraction can damage muscle fibers, especially if contractions are performed during lengthening. While obesity itself is not a contraindication, the ability to transfer the signal is a function of the resistance of the skin. For patients with extensive neck fat (the so-called double chin or turkey neck), it may be difficult to sufficiently overcome the resistance of the tissue for adequate signal transfer.
Characteristics of Electrical Stimulation
In order to adequately apply electrical stimulation, it is important that clinicians understand how to alter the characteristics of the electrical stimulation to achieve the desired result. Without this knowledge, clinicians become “knobologists” — individuals who merely follow a protocol by adjusting knobs to prescribed settings with limited understanding of how to manipulate settings for an individual patient and goal. See Box 4.42 for a brief summary of the characteristics to be discussed.
Box 4.42: Characteristics of electrical stimulation
|
Frequency |
Amplitude |
Waves |
Phase / Pulse Duration |
Duty Cycle |
|
Rate of pulses per second |
Intensity |
Monophasic, Biphasic, or Polyphasic |
Time to complete one phase or pulse |
The amount of time the signal is on versus off |
 |
 |
 |
 |
 |
Clinical Note
It has been hypothesized that for patients with head and neck cancer, electrical stimulation, if placed directly over a neoplasm may increase the spread of malignancy. However, this finding is not supported in the literature. Still it is reasonable to seek medical support from the oncologist before implementing an NMES protocol in this population.
Clinical Note
Motor recruitment patterns reverse with NMES. That means that larger fibers are recruited first, and smaller fibers are recruited last.
Clinical Note
There is debate regarding electrical stimulation of infrahyoid muscles as these lower the larynx. If this stimulation pattern is coupled with oral intake, the downward actions of the stimulation increase the risk of aspiration. However, if exercise tasks do not incorporate oral intake, then the downward pull can serve as a resistance to the desired upward movement which can be achieved with functional activity such as a saliva swallow.
Frequency
Frequency determines the number of electrical pulses per second (i.e., repetitions of the stimulus). Frequency is sometimes referred to as pulse rate. It is measured in Hertz (Hz). Changes in frequency will alter the firing rate and can be used to define the number of repetitions in a set. With consideration of patient tolerance, frequency is adjusted to get a desired response, such as a motor contraction if the goal is to stimulate a muscle fiber.
Phase / Pulse Duration
Phase duration is the time from the onset to the offset of the phase. Pulse duration, sometimes referred to as the pulse width, is the time form the onset of the first phase to the offset of the last phase of a single pulse. In a monophasic waveform, the pulse duration equals the phase duration. Pulse and phase duration are measured in time.
Amplitude
Amplitude refers to the intensity or strength of the delivered stimulus. It reflects the distance from the zero line to the peak in either direction. It can be adjusted to accommodate patient’s tolerance of the stimulus or to recruit a desired nerve. As shown in the strength-duration curve (Box 4.42), generally, sensory fibers become depolarized with lower current, while motor fibers require higher current. Pain fibers depolarize with greater amplitudes.
Frequency-Amplitude Relationship
There are specific frequency and amplitude combinations that can be used to stimulate different fiber types (motor, sensory, and pain). This relationship is represented in a strength-duration curve, which is simply a graph that represents that response to different intensities as a function of phase duration. In healthy nerves, at a given phase duration, sensory fibers are stimulated first, followed by motor fibers, and with increased amplitude, pain fibers.
Waveform
The waveform refers to the shape of the signal –monophasic, biphasic, or polyphasic (Box 4.42). While in other disciplines, protocols may incorporate various waveforms, currently, in our field, only biphasic waveforms are employed. A symmetrical biphasic pulsed wave is typically considered to be the most comfortable waveform when the goal is muscle strengthening.
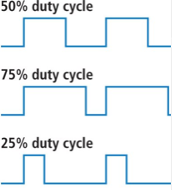
Duty Cycle
The duty cycle of a device indicates the work-rest ratio provided in the stimulation chain (Box 4.42). If a device indicates a duty cycle of 1:1, then for every unit of work there is an equal unit of rest. The duty cycle comprises the ramp up or rise time, which is the amount of time it take for the signal to reach its peak, and ramp down, which is the time it takes the peak amplitude to return to zero. The ramp up time may be adjusted to allow the patient to acclimate to the signal. Typically, a higher duty cycle fatigues the system more quickly. As fatigue or overload is required to effect change at the muscular level, when a duty cycle is biased such that it allows for recovery of the muscle, it will be difficult to achieve the needed fatigue to increase muscle strength.
Airway Protection
Airway protection may be improved by changing the strength, timing, or duration of airway closure. Any exercise that improves glottal valving, changes the onset of glottal closure, or alters the ability of the larynx to get out of the way of the bolus flow may translate to improved airway protection. Increasing the strength of the cough response may also improve airway protection.
Respiratory Muscle Strength Training
Respiratory muscle strength training can be used to improve strength in inspiratory or expiratory muscles. Of these, only expiratory muscle strength training (EMST) has been studied as a rehabilitative treatment for swallowing. The goal of the exercise is to increase expiratory muscle strength, which is hypothesized to translate to increased force generation during a cough. Briefly, if expiratory muscles can be strengthened and the increase in strength results in an increase in force generation during a cough, then airway invasion is more likely to be successfully expelled. The strength training is accomplished with the use of a device that contains an adjustable one-way spring-loaded valve to manipulate resistance.
Procedure
EMST entails quickly and forcefully blowing into the device where airflow is met with resistance and the force of the exhale is used to overcome that resistance. In the training protocol, a threshold for overcoming the resistance is established and adjusted as needed to maintain a progressive increase in the required muscle activity (Box 4.43). This threshold is re-evaluated and adjusted at regular intervals throughout the training program in order to maintain the relative resistance during exhalation. Using 75% of a patient’s maximal expiratory pressure, the trainer can be set and adjusted to maintain the relative resistance produced during the exercise task. Generally, training continues with weekly readjustment of the device for at least 5 weeks.
Box 4.43: Sample expiratory strength training protocol
- Minimum treatment length is not clear, but it is likely that a minimum of 4 weeks is needed to achieve the desired goal.
- Establish maximum expiratory pressure (MEP)
-
- This can be measured instrumentally or informally assessed by progressively increasing the resistance until he patient is unable to expel air through the device despite effort.
- MEP is reestablished each week.
- With the patient in seat
- ed position, nasal airflow is occluded with a nose clip.
- The resistance is set to approximate 75% of maximal expiratory pressure.
- Once the correct resistance setting is established the patient performs the exercise set.
-
- The patient blows hard and fast until the air rushes through the device then stops.
-
-
- The image of a blow-dart gun can be modeled to help the patient achieve a quick and hard exhale.
- This action is repeated 5 times to make a set with a rest period of at least 30 secs between each trial.
-
- The set is repeated 5 times a day, and this is completed 5 days a week.
Task Specific Modifications:
- Individuals can use their free hand to maintain cheek stability.
Efficacy
Based on available limited evidence, EMST can improve cough strength in elderly sedentary individuals, as well as individuals with spinal cord injury, degenerative neurologic disease such as Parkinson’s and multiple sclerosis, respiratory disease such as COPD, and post-stroke (Kim & Sapienza, 2005; Baker, Davenport, & Sapienza, 2005; Park, Oh, Chang & Kim, 2016; Troche et al., 2010; Chiara, Martin, Davenport, & Bolser, 2006). Any individual with dysphagia and a weak cough may be appropriate for this protocol. It may not be an ideal treatment for individuals prone to migraines or syncope, or individuals with degenerative muscle fiber disease such as muscular dystrophy or cystic fibrosis.
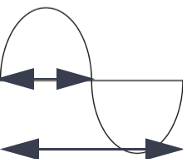
Respiratory Pattern Training
Recall that during a swallow there is a well-timed coordination between the respiratory and swallow systems (Martin, Logemann, Shaker, & Dodds, 1994; Martin-Harris et al., 2005). In healthy individuals, swallow typically occurs at the interface between inspiration and expiration, or early in the exhale and is followed by continued exhalation (Box 4.44). When the swallow is followed by inhalation there is an increased risk of penetration or aspiration (Brodsky et al., 2010).
Box 4.44: Respiratory- swallow timing
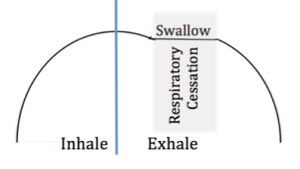
Guided by motor learning theory, the treatment is divided into three phases — identification of the desired respiratory-swallow pattern (during exhalation), learning and practicing the desired pattern, and automatic correct use of the pattern.
There is limited support that when respiratory-swallow pattern training is provided, then patients with head and neck cancer show a increase in tongue base retraction, improved closure of the laryngeal vestibule and reduced pharyngeal residue yielding an increase in swallow safety (Martin-Harris et al., 2015).

